The financial cost of missed appointments in the National Health Service (NHS) has been estimated at £360 million per year (Reference Stone, Palmer and SaxbyStone et al, 1999), most of this accounted for by non-attendance in primary care and hospital out-patient clinics. The purpose of this article is to review the extent and predictors of non-attendance in people with mental disorders presenting in primary and secondary care. Although one approach may be to fundamentally question the merits of out-patient clinics (Reference KillaspyKillaspy, 2006), our approach is to examine essential predictors and solutions within current models of care. In considering the classification of missed appointments it is important to distinguish between those who do not attend their first appointment and those who do not attend follow-up appointments. Unfortunately, in reviewing the literature few studies uphold this distinction. It is also useful to separate individuals who occasionally miss appointments (partial non-attendance) and those who disengage from any follow-up (often called treatment drop-outs). To put non-attendance in context, patients may experience difficulty following medical advice at each stage of their patient journey (Fig. 1).
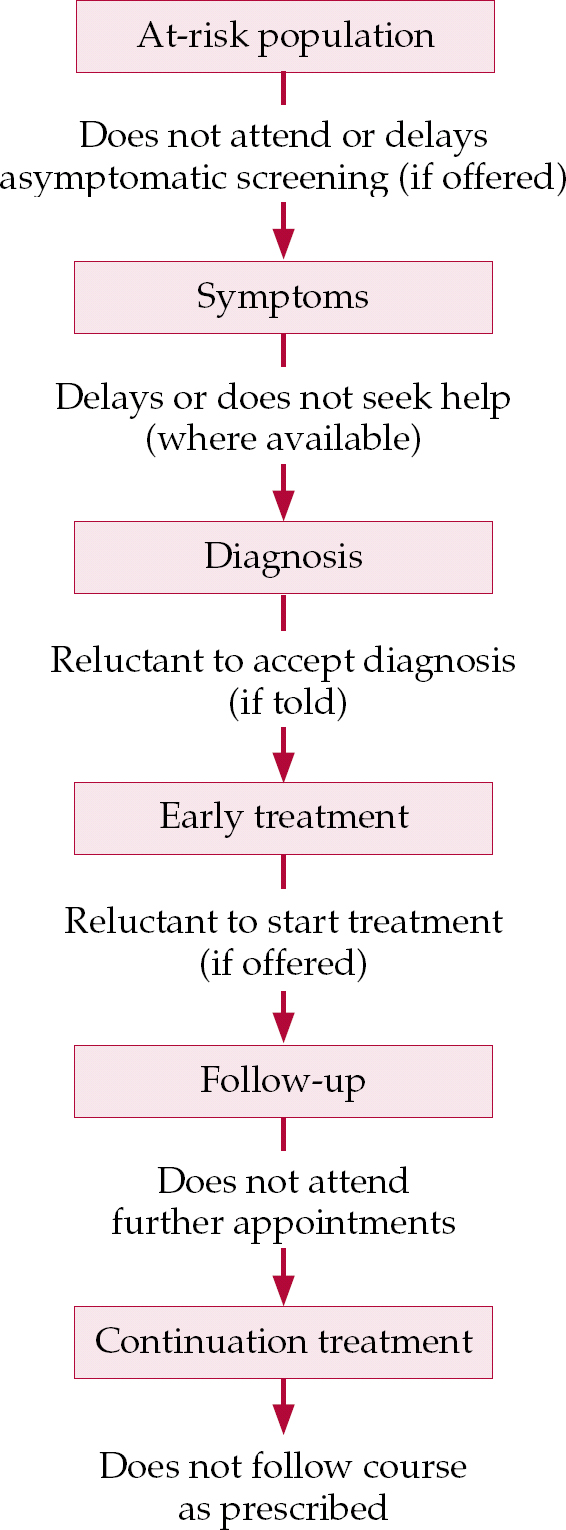
Fig. 1 Stages of difficulty in following medical advice.
The extent of non-attendance in psychiatry (and perhaps its impact on the patient) may be significantly greater than in other medical specialties. In 2002–2003, 19.1% of psychiatry out-patient appointments were missed in England, compared with an NHS-wide figure of 11.7% (Department of Health, 2003). Of note, the Commission for Healthcare Improvement (now the Healthcare Commission) showed that non-attendance rates varied more than fivefold across 83 mental health trusts in England (data collated from http://www.chi.nhs.uk/ratings). These national figures have been replicated in numerous small studies based in psychiatry out-patient clinics, which have reported non-attendance rates of 15.6–28% when examined as a proportion of all offered appointments (Reference Carpenter, Morrow and Del GaudioCarpenter et al, 1981; Reference Matas, Staley and GriffinMatas et al, 1992; Reference Dobscha, Delucchi and YoungDobscha et al, 1999; Reference Killaspy, Banerjee and KingKillaspy et al, 2000). Rates of initial non-attendance are usually higher than follow-up non-attendance, although this pattern may not hold for certain specialties (Reference Mitchell and SelmesMitchell & Selmes, 2007b ). The frequency of partial non-attendance is higher than the rate of full discontinuation (drop-out), echoing the findings of studies of missed medication (Reference Mitchell and SelmesMitchell & Selmes, 2007a ). Regarding partial non-attendance, Reference Akerblad, Bengtsson and EkseliusAkerblad et al(2003) in Sweden found that among 1031 patients with depression treated in primary care over a 6 month period only 54.6% of all scheduled appointments were kept. In the largest study of full disengagement, Reference Young, Grusky and JordanYoung et al(2000) found that 31% of community psychiatric patients were lost to follow-up over the course of 1 year. Over the course of 2 years the documented attrition rate for unscheduled drop-out may be as high as 50% (Reference Percudani, Belloni and ContiniPercudani et al, 2002).
Consequences of non-attendance in psychiatry
Non-attendance as a predictor of drop-out, relapse and readmission
An important question is how many of those who miss an appointment later reattend and resume treatment, and how many drop out of care permanently. Early non-attendance increases the risk of further non-attendance (Reference Carpenter, Morrow and Del GaudioCarpenter et al, 1981), but two prospective studies suggest that many patients who occasionally miss appointments subsequently reattend. Reference Sparr, Moffitt and WardSparr et al(1993) found that over a 3-month period 71.1% of missed appointments were rescheduled spontaneously by the patient (mostly within 2 weeks) and only about 25% resulted in disengagement from services. Reference Pang, Lum and UngvariPang et al(1996) traced 258 patients 6 months after their non-attendance at a follow-up clinic: 50% eventually returned but 50% dropped out of treatment. There is also good evidence that missed appointments, and unexpected disengagement in particular, can signal deteriorating mental health. In a prospective study of 365 out-patients receiving mental healthcare, Reference Killaspy, Banerjee and KingKillaspy et al(2000) found that follow-up patients who missed an appointment were more unwell and more functionally impaired than those who attended. In a comprehensive study, Reference Nelson, Maruish and AxlerNelson et al(2000) collected data on 3113 psychiatric admissions in eight south-eastern US states and calculated rehospitalisation rates after discharge. On the basis of the 365-day rehospitalisation rate, patients who kept a follow-up appointment had a 1 in 10 chance of being rehospitalised; for patients who did not keep (or were not offered) an appointment, the chances were 1 in 4. It is possible that the complications of non-attendance differ for new and ongoing patients. Reference Killaspy, Banerjee and KingKillaspy et al(2000) interviewed 57 new patients and 167 follow-up patients who did and did not attend general adult psychiatric out-patient clinic appointments over 12 months. Follow-up patients who did not attend had a 33% chance of being admitted in the next 12 months, compared with a 20% chance for the group that did attend. Also, the new patients who failed to attend were less likely to have agreed to the referral and less likely to have had it adequately explained to them.
A related concern is that attendance rates in those recently seen in emergency departments for self-harm who are offered follow-up are low (Reference Mitchell, Kingdon and CrossMitchell, et al, 2006). Indeed, the Confidential Inquiry into Homicides and Suicides by Mentally Ill People (Royal College of Psychiatrists, 1996) found that 28% of mentally ill suicide victims had lost contact with mental health services, 24% of suicides occurred within a month of discharge from hospital and most were before the first follow-up appointment had even taken place.
Attendance and medication adherence
Regular monitoring has been shown to lead to significant improvements in adherence to medication regimens (Fig. 2). When the US Federal Drug Administration decreased mandatory clozapine blood monitoring from weekly to every second week, there was a 10% rise in medication discontinuation (Reference Patel, Crismon and MillerPatel et al, 2005). As discontinuation of medication can lead to a significant deterioration in quality of life, it can be said that clinical contacts, medication use and quality of life are interrelated. Non-attendance is particularly closely linked with medication non-adherence (Reference Mitchell and SelmesMitchell & Selmes, 2007a ). Patients who discontinue medication of their own accord may be reluctant to disclose this to medical staff, and indeed cannot disclose it if not seen again. Conversely, patients who miss appointments will not receive the full benefit of medical advice and hence are less likely to make an informed choice about their care and are more likely to act autonomously in a self-directed manner (Reference MitchellMitchell, 2007).

Fig. 2 Illustration of the factors influencing adherence to medical advice.
Non-attendance and medical attitudes
Missed appointments may result in increased provider frustration (Reference Husain-Gambles, Neal and DempseyHusain-Gambles et al, 2004), decreased levels of provider empathy and lower quality patient–provider communication (Reference Pesata, Pallija and WebbPesata et al, 1999). In a primary care study, general practitioners (GPs) developed negative attitudes about patients who unexpectedly missed their appointments (Reference Husain-Gambles, Neal and DempseyHusain-Gambles et al, 2004). Not infrequently, favoured intervention strategies involve punishing the patient in some way for their ‘offence’ rather than discussing missed appointments with the patient (see also the section ‘Service responses to missed appointments’ below). Remarkably, despite the high risk of missed appointments in mental health services, a US survey showed that psychiatrists tended to be less active in trying to maintain contact with patients than non-physician therapists and junior doctors (Reference Smoller, McLean and OttoSmoller et al, 1998).
Predictors of non-attendance
Few studies have examined the predictors of non-attendance systematically in mental health settings (Reference ChenChen, 1991). In general, predictors may be divided into environmental and demographic factors, patient factors, illness factors and clinician factors (Box 1). The latter has been least investigated.
Box 1 Key predictors of non-attendance
Environmental and demographic factors
-
• Younger age
-
• Lower socio-economic status
-
• Not having health insurance (where health-care is not free at point of delivery)
-
• Poor adherence to psychotropic medications
-
• Homelessness
-
• Transport problems, distance from clinic
Patient factors
-
• Forgetting, oversleeping, getting the date wrong
-
• Being too psychiatrically unwell
-
• High trait anxiety
-
• Lower social desirability scores
-
• Dismissing attachment styles
Memory/cognitive problems
-
• Dementia
Information and health beliefs
-
• Poor insight into illness
Illness factors
-
• Personality disorder
-
• Substance misuse (alone or in combination with other psychiatric disorder)
-
• Neurotic disorders
-
• Diagnosis unclear or cannot be established
Clinician and referrer factors
-
• Poor communication between the referring practitioner and the patient
-
• Patient's disagreement with the referral
-
• Referrer's scepticism about the value of psychiatry
-
• Poor-quality referral letter
-
• Longer delay between the referral and the appointment (or between assessment and treatment)
-
• Early stages of treatment
-
• Quality of therapeutic alliance
-
• Non-collaborative decision-making
Environmental and demographic factors
A number of social and environmental factors have been linked to missed appointments in most medical specialties. Research indicates that patients who miss appointments tend to be younger and of lower socio-economic status (Reference Sharp and HamiltonSharp & Hamilton, 2001). Compared with attenders, such patients are more often in receipt of healthcare (incapacity) benefits and/or social benefits and are more likely to have psychosocial problems (Reference CosgroveCosgrove, 1990). In a comprehensive study of 221 000 primary care appointments in Sheffield, there was a strong correlation (r = 0.72) between non-attendance and the Townsend Deprivation Index Score for the patient's medical practice (Reference Waller and HodgkinWaller & Hodgkin, 2000). Reference Kruse, Rohland and WuKruse et al(2002) examined the medical records of 313 individuals with serious mental illness who were attending a US psychiatric out-patients clinic and found that 36% had missed their first appointment. The significant predictors were young age, Hispanic ethnicity, having a poor family support system, not having health insurance and also poor adherence to psychotropic medication (Reference Kruse, Rohland and WuKruse et al, 2002). In a study of 600 patients followed up after an emergency psychiatric assessment, Reference Dobscha, Delucchi and YoungDobscha et al(1999) found that homeless people were the least likely to attend, managing only a 34% follow-up rate. Although encouragement from family and friends is helpful, people who feel pressurised into attending by their family or doctor may be less likely to keep appointments.
A number of understandable accessibility issues are common to most studies of both help-seeking and attendance. Most frequently, transportation problems are cited (Reference Pesata, Pallija and WebbPesata et al, 1999), and distance travelled is another correlate (Reference Jackson, Booth and McguireJackson et al, 2006).
Patient factors
The most common single reason for non-attendance at follow-up appointments is forgetting the appointment, followed by being too psychiatrically unwell (Reference Killaspy, Banerjee and KingKillaspy et al, 2000). The proportion of psychiatric patients accidentally (unintentionally) missing an appointment appears to be higher than in other medical specialties. Reference Sparr, Moffitt and WardSparr et al(1993) examined reasons for non-attendance in 8.8% of 1620 contacts who missed scheduled appointments during a 3-month period. The most commonly stated reason for missing an appointment was patient error (forgetting, oversleeping or getting the date wrong). Reference Gudjonsson, Hannesdottir and AgustssonGudjonsson et al(2004) examined non-attendance in an alcohol clinic in Reykjavik. Of 313 patients asked to attend a follow-up appointment, only 27% did so. Predictors of non-attendance were younger age, high trait anxiety and lower social desirability scores. Psychoticism on the Eysenck Personality Questionnaire was the biggest single discriminator between those who attended. A study of the management of 3923 patients with diabetes in primary care found that those with secure attachment styles (as assessed by the Relationship Questionnaire) were significantly more likely to attend than those with dismissing attachment styles (Reference Ciechanowski, Russo and KatonCiechanowski et al, 2006). Reference Compton, Rudisch and CrawCompton et al(2006) collected data from team members and medical notes on 234 consecutively discharged patients from two in-patient units in a US urban county hospital. In a logistic regression model, the four characteristics that were significant predictors of missed first appointments were involuntary legal status at discharge or leaving against medical advice, not having an established out-patient clinician, an Axis IV problem relating to the patient's primary support group (for example, death of a family member or health problems in the family) and the number of days from discharge to the follow-up appointment.
Memory problems
Memory impairment may play a role in non-attendance as well as in subsequent engagement with treatment and services. Reference Rosen, Beauvais and RigsbyRosen et al(2003) examined the role of cognition in adherence behaviour in patients with diabetes. Low scores on the Mini-Mental State Examination and ‘non-Caucasian’ ethnicity were associated with missed appointments. Reference McKellar, Kelly and HarrisMcKellar et al(2006) found that greater cognitive dysfunction predicted drop out from treatment in a residential substance use disorder programme. This effect is not a reflection of old age itself, as older people have lower rates of non-attendance than younger patients (Reference Mitchell and SelmesMitchell & Selmes, 2007b ). A further concern with cognitive impairment is that it may affect a patient's ability to engage with a consultation or treatment programme – or indeed to subsequently recall the results of consultations. Reference Neupert and McDonald-MiszczakNeupert & McDonald-Miszczak (2004) studied 105 younger adults and 58 older adults who did not have a psychiatric diagnosis. Hierarchical regression results revealed that cognitive abilities and metacognitive beliefs were related to delayed recall of medication instructions. Dementia is an obvious reason for non-attendance but this has been inadequately studied (Reference Dockery, Rajkumar and ChapmanDockery et al, 2001).
Information and health beliefs
Several authors have observed that patients with schizophrenia who miss appointments are more likely to have lower levels of functioning, to be more severely unwell and also to have substance use problems (Reference Coodin, Staley and CortensCoodin et al, 2004). Yet, in depression and anxiety disorders, patients with milder disorders appear less likely to attend (Reference Issakidis and AndrewsIssakidis & Andrews, 2004). It is probable that a bimodal (U-shaped) relationship is present, with both the mildest and the most severe disorders linked with greatest non-attendance. Severity of illness and non-attendance may be mediated by insight. In a study of 33 patients with psychosis, poor scores on all commonly used insight assessment scales predicted poor adherence to treatment (Reference Sanz, Constable and Lopez-IborSanz et al, 1998). Most significantly, a large systematic review of 103 studies into clinic attendance and medication adherence in psychosis found an overall non-adherence rate of 25.8%. Predictors of non-adherence were lack of insight, positive symptoms, younger age, male gender, substance misuse, unemployment and poor social functioning (Reference Nose, Barbui and TansellaNose et al, 2003).
Illness type
Reference Matas, Staley and GriffinMatas et al(1992) reviewed the notes of 874 new out-patient referrals, and found that non-attendance was associated with a diagnosis of a personality disorder or substance misuse.
Reference Percudani, Belloni and ContiniPercudani et al(2002) found that in an Italian sample, patients with neurotic and personality disorders were more likely to drop out of treatment than those with schizophrenia. Similarly, Reference Young, Grusky and JordanYoung et al(2000) found that patients with schizophrenia were more likely to remain in contact with routine mental health services in Ventura County, California. Interestingly, if the diagnosis is unclear (or cannot be established) patients are more likely to drop out of care (Reference Melo and GuimarãesMelo & Guimarães, 2005).
Reference BellBell (2001) reviewed the evidence on factors influencing disengagement with treatment for bulimia nervosa. Although 28 studies were found, the only robust finding was that comorbid borderline personality disorder increased the likelihood of withdrawal from treatment. These differences are also reflected in different rates of non-attendance across services. We examined 17 211 out-patient psychiatric contacts across one calendar year and found a hierarchy of non-attendance (Reference Mitchell and SelmesMitchell & Selmes, 2007a ). Non-attendance rates for new patients ranged from 36.9% in alcohol services and 25.3% in drug services to 5.0% in the treatment and recovery (rehabilitation) service and 8.7% in liaison psychiatry. In most psychiatric subspecialties, the follow-up non-attendance rate was less than that for new patients. However, this pattern was reversed in child and adolescent psychiatry, drugs services, old age psychiatry and, most notably, liaison psychiatry, where the 8.7% of new-patient non-attendance rose to 20.9% at follow-up. Finally, many studies show that substance misuse complicates attendance. For example, Reference Sparr, Moffitt and WardSparr et al(1993) showed that patients with post-traumatic stress disorder and/or substance misuse were significantly more likely than others to miss appointments. In a study of 144 patients, Reference Ford, Snowden and WalserFord et al(1991) showed that those with comorbid substance misuse failed to keep 27.5% of scheduled appointments, compared with 15.8% of those with uncomplicated psychiatric disorders. In addition, the dual-diagnosis group had a drop-out rate almost three times higher than that of the single-diagnosis group.
Clinician and referrer factors
There is no doubt that the quality of service provided, as well as the rapport with the clinician, have a marked effect on attendance. Wilder et al(1997) suggest that ‘compliance’ is ‘as much a function of their [patients’] interactions with psychiatric personnel and of the suitability of the recommendations as it is of personal characteristics of the patients themselves’. In fact, this effect begins with the original referrer to secondary care.
Influence of the referrer
Poor communication between the referring practitioner and the patient may increase non-attendance at an initial appointment. Indeed, patients who agree with their referral are more likely to attend than those who do not (Reference Killaspy, Banerjee and KingKillaspy et al, 2000). General practitioner referrals to specialist care may result in a lower rate of attendance than those from other specialists (Reference Carpenter, Morrow and Del GaudioCarpenter et al, 1981). In a recent study (Reference Mitchell and SelmesMitchell & Selmes, 2007b ), we found that the rate of both initial and subsequent missed appointments was highest following self-referral and referrals from the police/probation service and lowest from community psychiatric nurses (CPNs), social services and from within psychiatric services. Reference Farid and AlapontFarid & Alapont (1993) found a remarkable association between non-attendance and a referrer who was sceptical about the value of psychiatry. There was also an association between the quality of the referral letter and the likelihood of attendance.
Influence of the assessor (primary clinician)
On a simplistic level, it is interesting to note that rates of missed appointments with consultants (clinical psychologists and psychiatrists) appear to be lower than those with trainees (Reference McIvor, Ek and CarsonMcIvor et al, 2004). Rates of initial non-attendance also increase with time when there is a delay between the referral (or scheduling) and the actual appointment (Reference Grunebaum, Luber and CallahanGrunebaum et al, 1996; Reference Gallucci, Swartz and HackermanGallucci et al, 2005). In the same manner, rates of follow-up non-attendance increase with delay between assessment and treatment (Reference Jackson, Booth and McguireJackson et al, 2006). Several studies suggest that patients are most likely to drop out during the early phase of treatment. For example, 69% of losses to treatment occurred in the first month in one study in Brazil (Reference Melo and GuimarãesMelo & Guimarães, 2005).
However, it is also useful to look at communication and interpersonal variables in more detail, utilising studies across medicine, as many clinicians will feel they have more control over communication style than scheduling delays. Perhaps the most important interpersonal variable in predicting attendance is the quality of the therapeutic alliance and, more specifically, the degree of ‘helpfulness’ of the health professional as perceived by the patient (Reference Johansson and EklundJohansson & Eklund, 2006) (Box 2). That said, in some studies clinician-rated alliance is a stronger predictor of drop-out than patient-rated therapeutic alliance (Reference Meier, Donmall and McelduffMeier et al, 2006). Willingness to discuss mental health issues with a doctor is also predicted largely by the perceived helpfulness of that doctor, and in turn trust in the doctor and the medical profession.
Box 2 Hypothetical patient's perspective of non-attendance
Anna experiences a racing heartbeat and wonders whether it is something medically serious or perhaps due to anxiety. She decides to call the GP for an appointment. The last time she had felt like this the GP had advised her to ‘wait and see if things got worse’, which did not seem very helpful but the symptoms did go away. The only available appointment is in 5 days’ time; Anna feels that the staff are not treating her concern seriously, but accepts the appointment because she is concerned. She begins to worry that the palpitations might cause a heart attack. Then she starts to worry what kinds of tests the doctor is going to perform; she is sure any tests will be uncomfortable and worries that they might show something serious. Both make her nervous about attending. After a few days she becomes less worried and the palpitations go away. Finally, thinking that her condition must not be serious, she decides not to keep her appointment. She is not sure that the GP could have helped anyway. She does not bother to telephone and tell the clinic because they are so busy they will not even notice her absence and will probably see someone else in her place. Also it might give the doctor 10 minutes to catch up on their work (because they always seem to be in a rush to finish).
Adapted from Reference Lacy, Paulman and ReuterLacy et al, 2004
Although trust and helpfulness are rarely measured routinely, satisfaction may be a proxy measure. Global dissatisfaction with care is a strong predictor of dropping out of care in most (Reference PekarikPekarik, 1983; Reference Tehrani, Krussel and BorgTehrani et al, 1996; Reference Young, Grusky and JordanYoung et al, 2000; Reference Rossi, Amaddeo and BisoffiRossi et al, 2002) but not all (Reference Killaspy, Gledhill and BanerjeeKillaspy et al, 1998) studies. However, satisfaction may be good with some aspects of care and poor with others. One study found that dissatisfaction with the skills and behaviour of health professionals and satisfaction with received treatment both predicted drop-out, suggesting that satisfaction with quality of care and satisfaction with treatment success should be separated (Reference Rossi, Amaddeo and BisoffiRossi et al, 2002).
Other work suggests that satisfaction is related to a patient-centred communication style and a willingness to forge an agreed therapeutic strategy (Reference Nakanishi, Koyama and ItoNakanishi et al, 2006). Yet patients are not always involved fully in treatment decisions. In one study, for example, only 1 in 10 patients taking clozapine remembered discussing potentially serious haema-tological effects (Reference Angermeyer, Loffler and MullerAngermeyer et al, 2001). The majority of patients taking antipsychotics do not feel involved in their treatment, and simply take their medication because they are asked to do so (Reference Gray, Rofail and AllenGray et al, 2005). A collaborative decision-making communication style (as reported by patients) was shown in a survey of 100 users of antidepressants to predict attendance and medication use (Reference Bultman and SvarstadBultman & Svarstad, 2000).
Conversely, bad experiences of health services have been linked with non-attendance. Reference Gonzalez, Williams, Noel and LeeGonzalez et al(2005) in Texas looked at adherence to appointments and medication in 95 combat veterans prescribed antidepressant medication, observed over 6 months. Appointment attendance was best in those who felt ready for treatment, perceived its benefits, had fewer negative effects from previous mental health treatment and saw their physician as collaborative. Patients who receive appointments after greater delay or who feel that the healthcare professional did not listen to, respect or understand them, are less likely to reattend (Reference Moore, Sickel and MalatMoore et al, 2004).
Interventions to reduce non-attendance
Reviews are available of methods of improving engagement in psychotherapy (Reference Ogrodniczuk, Joyce and PiperOgrodniczuk et al, 2005) and in adult mental health and substance misuse settings (Reference Lefforge, Donohue and StradaLefforge et al, 2007). In addition, Reference Macharia, Leon and RoweMacharia et al(1992) identified 23 randomised controlled trials in mixed settings which used attendance as the primary outcome measure. Written and telephone prompts positively influenced attendance. A more recent Cochrane review (Reference Reda and MakhoulReda & Makhoul, 2001) found evidence that a telephone or written prompt delivered 24 h before a clinic appointment may encourage attendance. A national campaign ‘Keep it or cancel it’, organised by the UK government-funded Developing Patient Partnerships Agency, was accompanied by £20 million in funding for a new computerised booking system (BBC, 1999). The cost-effectiveness of enhanced engagement methods has been questioned (Reference Sharp and HamiltonSharp & Hamilton, 2001), leading to several economic cost–benefit analyses. It may be useful for the following section to consider patient's reasons for non-attendance in two roughly equal categories: avoidable reasons such as forgetting, communication problems and transport problems, and unavoidable reasons such as illness relapse and illness remission. Interventions have been mainly aimed at the so-called avoidable factors.
Reminder and memory aids
The discovery that psychiatric patients are twice as likely to cite forgetting as the cause of non-attendance than those in other specialties (Reference Killaspy, Banerjee and KingKillaspy et al, 2000) might support interest in active reminder systems. Reference Boswell, Brauzer and PostlethwaiteBoswell et al(1983) was one of the first to use a telephone reminder before psychiatric clinic appointments for 184 patients compared with 185 treated as usual. There was a statistically significant improvement in attendance in this early randomised controlled trial. Similar positive results have since been reported for first attenders by Reference Burgoyne, Acosta and YamamotoBurgoyne et al(1983), Reference MacDonald, Brown and EllisMacDonald et al(2000) and Reference Conduit, Byrne and CourtConduit et al(2004), and for both first attenders and follow-up patients by Reference Shivack and SullivanShivack & Sullivan (1989) and for follow-up patients by Reference Bamford, Booth and McguireBamford et al(2004), the latter using both telephone and postal reminders with alcohol misusers. Telephone reminders seem to be particularly effective for elderly patients, especially those with dementia (Reference Dockery, Rajkumar and ChapmanDockery et al, 2001). Messages left on an answerphone can also be successful (Reference Conduit, Byrne and CourtConduit et al, 2004). Reference McFall, Malte and FontanaMcFall et al(2000) conducted a pilot outreach intervention for combat veterans receiving disability benefits for post-traumatic stress disorder but not receiving treatment. A letter inviting them to seek help followed by a telephone reminder led to a 23% attendance rate compared with 7% attendance for those who received just a letter. In one study of 103 new out-patients at a London psychiatric teaching hospital, patients were asked to confirm in writing or by telephone if they still required an appointment (Reference BaggaleyBaggaley, 1993). A number of automated methods of sending reminders to patients about scheduled appointments have been developed. For example, Reference Andrade, Mcgruder and WuAndrade et al(2005) measured the effect of a memory-prompting device (Disease Management Assistance System) on adherence to treatment in people with HIV. Interestingly, adherence improved only in those with diagnosed memory impairment. Unfortunately, the expense of these systems usually proves prohibitive for the majority of patients and healthcare providers.
Interpersonal and communication issues
Simple measures such as providing patients with sufficient information about the practical aspects of their appointment (where to park, directions, etc.) and even ‘orientation statements’ (explaining what to expect in the consultation) can lead to improvements in attendance (Reference Kluger and KarrasKluger & Karras, 1983). Reference Wenning and KingWenning & King (1995) offered the parents of children newly referred to child psychiatry an ‘orientation group meeting’, in which they were informed about the service provided. This reduced non-attendance at the first (but not subsequent) clinic appointments, and also allowed parents who were unlikely to attend to be identified in advance. Patients’ understanding can be increased with a simple discharge or exit interview explaining the need for follow-up and the rationale for medication. This approach appears to reduce subsequent non-attendance (Reference Guse, Richardson and CarleGuse et al, 2003). Given that one of the most important interpersonal variables in predicting attendance is the degree of helpfulness of the health professional (see above) we suggest that all clinicians check whether there is anything further that can be done to help at the close of all appointments and prior to hospital discharge. Even greater insight may be gained by routinely using an instrument to check the quality of their therapeutic relationships (Reference McGuire-Snieckus, McCabe and CattyMcGuire-Snieckus et al, 2007).
Service responses to missed appointments
All services must carefully consider their approach to those who miss one or more appointments (Reference Cruz, Cruz and McEldoonCruz et al, 2001). Clearly, many patients miss a single appointment by mistake (unintentionally) and we suggest that after one missed appointment a reminder is sent to the patient with another appointment date (or at least the offer of an appointment), possibly suggesting a home visit. After a second and third consecutive unexplained miss, there is a higher chance that the patient is unwilling or unable to attend. We suggest speaking directly to the patient, clarifying whether an appointment is still needed and, if so, finding a mutually agreed time. If a patient cannot be contacted an alternative is to ask the referrer to clarify whether the appointment is still wanted. Simply sending three written appointments for fixed out-patient slots may not be satisfactory as there is no allowance for administrative error or severe illness. An important question that arises when a patient is initially seen but then disengages is whether that service was truly meeting the individual's needs. It is not uncommon for patients to drop out of treatment because of a perceived lack of progress. For this reason we suggest attempting to ask all patients who disengage for feedback either verbally or in writing.
It is vital that services in all specialties review the ongoing needs of the patients they serve. For example, when staff at a paediatric clinic noted a particularly high non-attendance rate among Asian patients (50%) they found that common-sense steps, including avoiding appointments during Islamic religious festivals, reducing language barriers through the use of link workers, liaison with elders and education of staff, reduced this figure to 13.5% (Reference GatradGatrad, 2000). Surveys of non-attending patients (as described above) show that people often view services as inaccessible (and, to a lesser extent, inflexible). Although it is uncommon for patients to cite problems with the appointment time as a reason for non-attendance, significantly more patients will attend afternoon than morning appointments (Reference Weinerman, Glossop and WongWeinerman et al, 2003). In a study of 118 substance-misusing young people, a community-based treatment programme that was much easier to access than conventional care reduced disengagement from 22% to 2% (Reference Henggeler, Pickrel and BrondinoHenggeler et al, 1996). However, flexible but complex systems risk alienating those who cannot read English, or who have intellectual disabilities or significant psychiatric morbidity (Reference Sharp and HamiltonSharp & Hamilton, 2001).
The effectiveness of providing evening and weekend appointments has not been investigated in mental health settings, but providing hospital transport or taxis is beneficial (reducing non-attendance at prenatal appointments for low-income women by 22%) (Reference Melnikow, Paliescheskey and StewartMelnikow et al, 1997). The innovative but controversial method of rewarding those who attend clinic and/or punishing those who do not has been successfully piloted by more than one group (Reference Parrish, Charlop and FentonParrish et al, 1986; Reference BechBech, 2005). It may be more ethically acceptable to offer a nominal reward option alone (‘as a thank you for letting us know you could not attend’) (Reference Pollastri, Pokrywa and WalshPollastri et al, 2005).
Assertive outreach and home treatment services
A minority of patients find engagement with hospital-based services difficult or impossible. They may have a history of disengagement leading to hospital admissions. In the past two decades, dedicated assertive outreach teams have been set up in the UK with the aim of engaging with patients and reducing hospital admission. The model of assertive outreach includes long-term engagement, shared case-loads and flexibility (Sainsbury Centre for Mental Health, 2001). There is evidence that this approach is accompanied by a significant improvement in patient engagement (Reference WharneWharne, 2005). Home treatment alone may also have demonstrable benefits, although not necessarily in rates of rehospitalisation (Reference Frederick, Caldwell and RubioFrederick et al, 2002). Of course, these principles can equally be applied in routine settings and for other types of patient. It may be advantageous to engage with patients who have cognitive impairments in their own home. In a 4-year study of out-patient old age psychiatry in an urban area of the UK, home visits had a much lower ‘non-attendance’ rate (1.7%) than clinics (21.2%) (Reference Anderson and AquilinaAnderson & Aquilina, 2002).
Conclusions
There are many reasons for missed appointments, most often slips and lapses (e.g. forgotten appointments), and in many cases patients will later reattend without adverse consequences. However, an important proportion will not reattend and deteriorate without accessing further medical help. Both missed appointments and missed medication may herald disengagement (dropout) from care. Faced with non-attendance it is difficult for clinicians to know which category (no help needed or at risk) individual patients fall into. For this reason a policy of discharge after one or more missed appointments may not be appropriate without clarification of need. Non-attendance due to barriers to care and administrative errors is not uncommon and can often be improved (Reference Stone, Palmer and SaxbyStone et al, 1999). Systematic changes in appointment systems can reduce barriers to help-seeking and hence reduce non-attendance. It is important to recognise that non-attendance is not limited to those with psychotic disorders who lose insight: in fact, patients with schizophrenia may engage more successfully than other groups with mental illness (Reference Young, Grusky and JordanYoung et al, 2000; Reference Percudani, Belloni and ContiniPercudani et al, 2002).
Patient surveys reveal that most people feel anxious about seeing a doctor, especially a psychiatrist and/or when potentially receiving ‘bad news’ (Reference Grunebaum, Luber and CallahanGrunebaum et al, 1996). Teams can do much to alleviate this anxiety – and hence large improvements in missed appointment rates can be achieved by relatively simple measures (Box 3).
Box 3 Simple measures to reduce non-attendance
Improving initial attendance
-
• Encourage referrers to explain the purpose of the referral
-
• Schedule the appointment as soon as possible
-
• Write to the patient with clear directions and explaining the mechanism of referral
-
• Offer the option of an afternoon appointment
-
• Offer the option of a community/home visit if the patient is too unwell to attend
-
• Consider a reminder telephone call the day before the appointment (if the patient has a telephone)
Improving follow-up attendance
-
• Give the patient a choice of appointment dates and/or locations
-
• Schedule the appointment as soon as possible
-
• Where possible, agree the duration of the treatment course at the start
-
• Work towards establishing and maintaining a good therapeutic relationship
-
• Involve the patient in treatment decisions
Response to missed appointments
-
• Contact the patient by letter or telephone
-
• Identify any patient-cited barriers to attending
-
• Confirm that the patient wishes to attend
-
• Affirm that the patient can still be seen without prejudice
-
• If possible convey hope that there is a definite prospect of improvement
-
• Reschedule the missed appointment as soon as possible
(Adapted from Reference Pettinati, Weiss and MillerPettinati et al, 2004)
A valid question is why many do not ring to cancel rather than missing an appointment. Preliminary data suggest that a third forget or do not consider cancelling and may be too embarrassed on the day to call to admit this, and a small but important group are too unwell and/or cannot easily ring on the day (Reference HamiltonHamilton, 2001). Another important reason for non-attendance is problems in the therapeutic alliance. These issues are often ignored, perhaps because health professionals are uncomfortable examining their own practice. However, simple measures of clinician- and patient-rated therapeutic alliance are available. High non-attendance rates are sometimes a marker that aspects of quality of care could be improved. There appears to be an important difference between psychiatry patients who miss their first appointment and those who miss a follow-up appointment. The first appointment is heavily influenced by an individual's pre-existing health beliefs and the quality of the information given by the first referrer. Attendance at follow-up appointments is a reflection both of the patient's overall satisfaction with care and the perceived need for further help (Box 2).
There appears to be a bimodal relationship between severity of illness and attendance. Low and high illness severity predict non-attendance. In other words the most common reason for not attending a first appointment is feeling better but the most serious is feeling too unwell (Reference CosgroveCosgrove, 1990).
We suggest that all health professionals consider barriers to care and attempt to contact patients directly before discharging those who do not attend without explanation.
Declaration of interest
None.
MCQs
-
1 Regarding non-attendance at psychiatric out-patient clinics:
-
a it is typically less serious than in other medical specialties
-
b non-attendance following hospital admission predicts subsequent readmission
-
c in most psychiatric specialties, follow-up patients are less likely to attend than those who are being seen for the first time
-
d a missed appointment most commonly heralds complete disengagement from mental health services
-
e most cases of missed appointments are due to loss of insight.
-
-
2 Psychiatric patients who fail to attend an initial clinic appointment:
-
a are generally less unwell than those who do attend
-
b may be assumed to be of low risk of suicide
-
c are more likely to adhere to medication regimens
-
d will be more likely to attend in the future if contacted by telephone
-
e should be discharged without follow-up, to avoid wasting NHS resources.
-
-
3 The following groups have relatively high rates of non-attendance:
-
a older people
-
b people given a rapid appointment
-
c those who score highly for neuroticism on the Eysenck Personality Questionnaire
-
d patients who misuse alcohol and drugs
-
e people from higher socio-economic groups.
-
-
4 Referrals made by the following groups have been associated with consistently good attendance rates:
-
a community psychiatric nurses
-
b the probation service
-
c patients themselves (self-referral)
-
d general practitioners
-
e professionals who perceive psychiatry negatively.
-
-
5 The following potential interventions to increase attendance have no evidence-based support:
-
a telephone reminder calls
-
b ‘orientation statements’
-
c assertive outreach services
-
d sending three repeat appointments by post
-
e memory aids for people with cognitive impairment.
-
MCQ answers

| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | F | a | F | a | T | a | F |
| b | T | b | F | b | F | b | F | b | F |
| c | F | c | F | c | F | c | F | c | F |
| d | F | d | T | d | T | d | F | d | T |
| e | F | e | F | e | F | e | F | e | F |







eLetters
No eLetters have been published for this article.