As the proportion of the population that survives to old age increases, we might expect to encounter more frequently in this group psychiatric conditions more commonly associated with early and middle adulthood. With this in mind, we have been interested in examining what is known about the prevalence and management of personality disorders among older people (65 years of age and above).
Personality and age
Although one's core personality is thought to remain stable over the adult years, modest variation may arise in terms of its expression with advancing age. For instance, an increase in obsessive–compulsive traits is common among older people and may reflect not so much a change in intrinsic personality as an adaptation of the person to failing powers or altered relationships and environments (Reference Engels, Duijsens and HaringsmaEngels et al, 2003). The neurological substrate of reduced adaptability has also been variously investigated in the context of cerebrovascular pathology (Reference Stone, Townend and KwanStone et al, 2004) and falling levels of central neurotransmitters (e.g. dopamine; Reference Volkow, Gur and WangVolkow et al, 1998).
Personality disorder (Box 1) is a controversial concept but the diagnosis remains pertinent in older people provided that a suitable account of long-standing dysfunction can be established that pre-dates presentation. In simple terms, personality disorder may be construed as a long-standing pattern of maladaptive interpersonal behaviour (Reference KroesslerKroessler, 1990). So, although it might be considered very late for the condition to present in old age (perhaps marking the culmination of many unhappy events for the individual) there might at least be the advantage of a considerable longitudinal history and pattern of behaviour for the examiner to investigate at the time of assessment.
Box 1 Diagnostic categories of personality disorder
DSM–IV (American Psychiatric Association, 1994)
Cluster A: ‘eccentric’
-
• Paranoid
-
• Schizoid
-
• Schizotypal
Cluster B: ‘flamboyant’
-
• Antisocial
-
• Borderline
-
• Histrionic
-
• Narcissistic
Cluster C: ‘anxious’
-
• Avoidant
-
• Dependent
-
• Obsessive–compulsive
ICD–10 (World Health Organization, 1992)
-
• Paranoid
-
• Schizoid
-
• Dissocial
-
• Emotionally unstable
-
• Histrionic
-
• Anankastic
-
• Anxious
-
• Dependent
Box 2 Barriers to diagnosis
-
• Lack of co-informant
-
• Co-informant with little knowledge of patient's early life
-
• Unreliable patient and/or co-informant
-
• Cognitive impairment of patient and/or co-informant
-
• Co-informant's characteristics (e.g. shame, minimisation, embarrassment, guilt) affect their account
-
• Severe physical illness in patient
-
• Axis I and Axis II similarities, e.g. paranoid personality disorder v. paraphrenia; dissocial personality v. frontotemporal dementia
Prevalence
There are relatively few prevalence data concerning personality disorder in older people, yet ICD–10 asserts that such disorders are stable and enduring over time (World Health Organization, 1992: p. 200). Hence, by inference, personality disorder ‘should’ be seen among this stratum of the population. However, as age advances, certain ‘problem’ behaviours associated with personality disorder (e.g. impulsivity, aggression, promiscuity, fighting and law-breaking) might be expected to decline in frequency, while comorbid psychiatric disorders might enhance the expression of other dysfunctional traits: there is, for instance, a predominance of social withdrawal and major depressive and dysthymic disorders among older people (Reference DevanandDevanand, 2002).
The prevalence of personality disorder among older people in the community has been estimated to be about 10% (Box 1) (Reference Abrams and HorowitzAbrams & Horowitz, 1996).
Among older in-patients, personality disorder has been described in 6% of those with organic mental disorders and 24% of those with major depressive disorder (Reference Kunik, Mulsant and RifaiKunik et al, 1994). In this sample, cluster C personality disorders (mainly the anxious and dependent types) were again more common. Patients with early-onset depression were more likely to exhibit personality dysfunction, mainly avoidant, dependent and ‘not otherwise specified’ (Reference Kunik, Mulsant and RifaiKunik et al, 1994; Reference Abrams and HorowitzAbrams & Horowitz, 1996). There is also some evidence that among older patients with major depressive disorder, personality disorder is associated with a recurrent pattern of (depressive) illness (Reference Kunik, Mulsant and RifaiKunik et al, 1994).
A further study, of 76 older people with dysthymia, found 31% (24) to have personality disorder. Of these, 17% (4) had obsessive–compulsive personality disorder, 12% (3) had avoidant personality disorder and 5% (1) had borderline personality disorder (Reference Devanand, Turret and MoodyDevanand et al, 2000).
As alluded to above, there is thought to be a reduction with age in certain dissocial behaviours and a possible decline in cluster B personality disorders (Box 1). If true, such a decrease might be attributable to:
-
• a reduction in dramatic behaviour intrinsic to ageing
-
• age-related neurobiological changes that affect the manifestation of dissocial conduct
-
• increasing physical incapacity, reducing the ability to ‘act out’
-
• attrition (through death) of those who have died by suicide or from other causes connected with personality disorder (e.g. recklessness)
-
• omission from studies of older people with antisocial personality disorder who are in prison or forensic psychiatric hospitals (Reference Fazel, Hope and O'DonnellFazel et al, 2001)
-
• a cohort effect, whereby older age groups derive from cohorts who had lower (pre-existing) levels of personality disorder than their younger comparators.
It is also possible that the natural history of the disorder is one of gradual improvement. Certainly, there is an anecdotal belief that certain personality disorders, for example borderline personality disorder, may ‘burn out’ with age. Indeed, the outcome of the latter is generally better than may be routinely acknowledged (Reference StoneStone, 1993). Two-thirds are clinically well at follow-up, although they may retain mild residual symptoms (Reference Stone, Hurt and StoneStone et al, 1987). One study found that only one-quarter of people with an initial diagnosis of borderline personality disorder retained this full diagnosis at long-term follow-up (Reference Zanarini, Frankenburg and HennenZanarini, 2003). As the individual ages, it seems that impulsivity resolves first; next to improve is interpersonal functioning, and affective symptoms are the last to reduce or disappear.
Personality disorder among older prisoners in England and Wales has been studied by Reference Fazel, Hope and O'DonnellFazel et al (2001). The prevalence was 30% (in total), with avoidant and antisocial categories contributing most (8.3% each), followed by anankastic (7.9%), schizoid (6.4%) and paranoid (3.4%).
Personality disorder as a risk factor for abuse
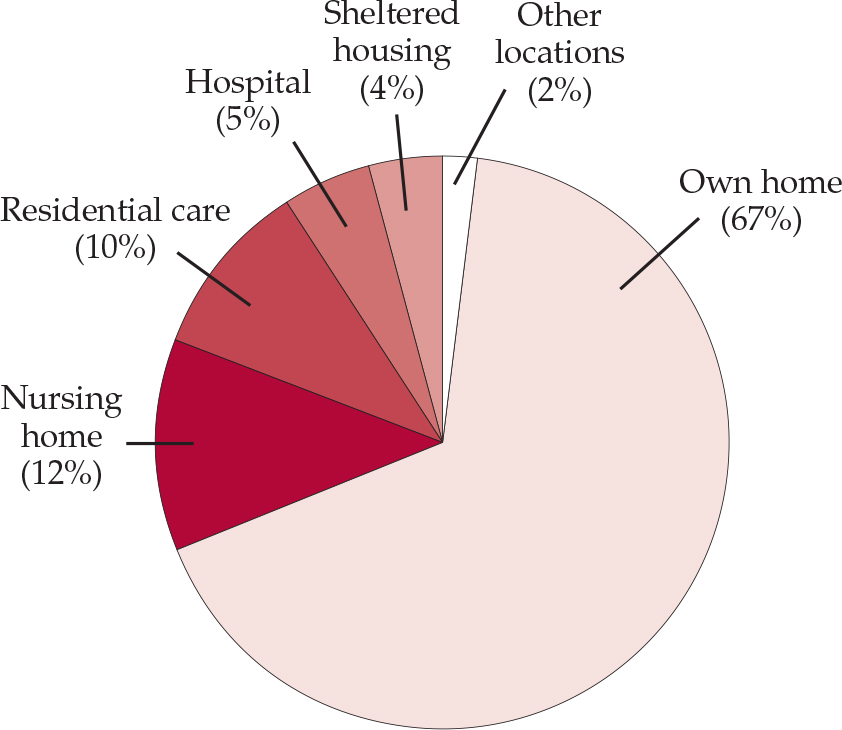
If someone has a difficult personality, does this place them at increased risk as they become older and perhaps infirm? Of the potential risk factors for elder abuse identified by the House of Commons Health Committee (2004) identified, social isolation and a poor relationship with a carer might reflect personality difficulties; others, however, relate more to the perpetrator than the victim, for example dependence of the abuser on the person they abuse and a history of mental health problems, personality disorder, or drug and alcohol problems in the abuser. Although the public perception might be that older people are at greater risk of abuse in residential and nursing care, over two-thirds of elder abuse happens in the victims' own homes (Fig. 1).
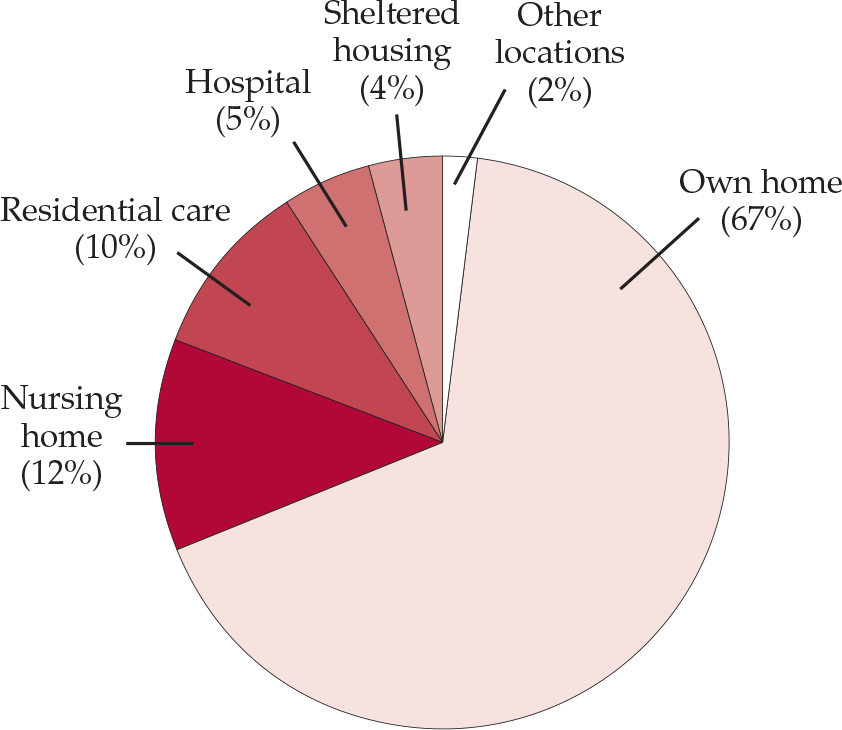
Fig. 1 Place of residence of people subjected to elder abuse in the UK (House of Commons Health Committee, 2004).
Older people with anxious and dependent personality disorders may be particularly prone to abuse (Reference Kurrle, Sadler and CameronKurrle et al, 1991), as are people undergoing organic personality change (Reference Hansberry, Chen and GorbienHansberry et al, 2005). This may be due to their disinhibition, inability to communicate and/or lack of decisional capacity.
Comorbidity associated with personality disorder
Personality disorder is often associated with an Axis I psychiatric disorder, and this may compound problems for the potential patient and their carer(s). The link between depression and personality disorder seems well established (Reference DevanandDevanand, 2002). Also, many patients with late-onset schizophrenia have never married, live alone and may have exhibited abnormal premorbid personality traits (Reference FuchsFuchs, 1999).
Affective disorder
Consistent data suggest that there is a strong relationship between personality disorder and depression. A case example is described in Box 3. The rate of personality disorder with a comorbid diagnosis of major depression was 24% in one study (Reference Kunik, Mulsant and RifaiKunik et al, 1994). In older people with personality disorder, there is a high rate (73%) of adult-onset rather than late-onset (geriatric) depression (45%) (Reference Camus, de Mendonca Lima and GaillardCamus et al, 1997).
Box 3 Personality disorder and depression: a case example
A 69-year-old widow was referred for depressive symptoms following social stressors (a son had emigrated). She had shown little response to antidepressants prescribed by her general practitioner.
It transpired that she had withheld information regarding contact with psychiatric services in early adult life for recurrent self-harm (lacerations to her wrists).
Placing her recent stressors in the context of her longer-term problems helped her to adjust (she had experienced separations before and survived).
Her antidepressant medication was adjusted and she received follow-up with the mental health team. Her depression responded well and she returned to independent living.
In a sample of older patients with dysthymic disorder, a personality disorder co-occurred in a minority and mainly comprised the obsessive–compulsive and avoidant subtypes (Reference Devanand, Turret and MoodyDevanand et al, 2000).
Anxiety disorder
Anxiety is a frequent concomitant of depression. Individuals with cluster C personality disorders seem more prone to developing anxiety disorder, phobias and acute stress disorder. Reference Sanderson, Wetzler and BeckSanderson et al (1994) examined personality disorder in 347 patients with anxiety disorder and found that the most common were avoidant (13%), obsessive–compulsive (11%) and dependent (8%) subtypes.
Somatisation disorder
Two-thirds of older people with depression have hypochondriacal ideas (De Alarcon, 1964); the main preoccupation being their bowels. In 30% of these patients, hypochondriacal ideas (somatic concern or hypochondria) precede depressive symptomatology.
Substance misuse
Certain personality disorders, especially those in clusters B and C, are more likely to involve problem alcohol use. In a study by Reference Speer and BatesSpeer & Bates (1992), it was found that older people are more likely to have the ‘triple diagnosis’ of personality disorder, alcohol dependence and depression.
Diogenes syndrome
Some people consider Diogenes syndrome to be an end stage of personality disorder. It refers to extreme self-neglect, unaccompanied by a medical or psychiatric condition sufficient to account for the condition. It can be seen as the response of someone with a particular personality type to old age and loneliness. It might also be a reaction to stress in older people with certain personality characteristics such as the schizotypal or anankastic (Reference Rosenthal, Stelian and WagnerRosenthal et al, 1999).
Dementia
Of course, personality changes occur in organic disorders even if they are not classified as personality disorder. Changes such as apathy and dysphoria have been described in Alzheimer's disease (Reference Landes, Sperry and StraussLandes et al, 2005). Frontotemporal dementia is characterised by personality changes such as lack of insight, apathy and disinhibition. Not all individuals experience such change, but in those that do three patterns have been reported: change at the onset of dementia; ongoing change with disease progression; and change into disturbed behaviour (Reference Petry, Cummins and HillPetry et al, 1989). Carers often describe personality changes such as becoming ‘out of touch’, reliant on others, childish, irritable, unreasonable, unhappy, cold and cruel (Reference Wattis, Butler and PittWattis, 1998). Some of these features may be attributable to organic changes, whereas others are a reaction to dementia. It is also possible that the dementing process ‘releases’ underlying behavioural propensities that the patient may have been better able to control when well.
Management of personality disorder
There is a very sparse literature on the management of personality disorder in older people: the basic principles are listed in Box 4. However, as mentioned earlier, personality disorder is commonly accompanied by an Axis I disorder, and judicious treatment of the latter may ameliorate certain aspects of the personality disturbance.
Box 4 Principles of treating personality disorder
-
• Form a therapeutic alliance
-
• Treat any comorbid Axis I disorder
-
• Adopt a consistent approach
-
• Use supportive cognitive psychotherapy
-
• Establish good links with other professionals
-
• Involve significant others where possible
Role of medication in treatment
Medications are often used to treat the functional illnesses comorbid with personality disorders.
The mainstays of pharmacological treatment of depressive disorders are obviously the anti-depressants. However, because of the frailty and physiological changes that occur with age, they are often started at low doses and increased slowly. The most commonly used antidepressants are the selective serotonin reuptake inhibitors (SSRIs), owing to their safer side-effect profile and less frequent interactions with other medications. Reference Kunik, Mulsant and RifaiKunik et al (1994) reported that older in-patients both with and without personality disorder who had major depression benefitted equally from treatment, primarily anti-depressant medication or electroconvulsive therapy (ECT). Conversely, Reference Thompson, Gallagher and BreckenridgeThompson et al (1987) found that concomitant personality disorder in older patients with major depression decreased the likelihood of response to psychotherapy.
Low-dose antipsychotic drugs are mainly used to control agitation and psychotic symptoms (Reference Bouman and PinnerBouman & Pinner, 2002). Their appropriate use in older people has become an area of increasing debate: typical antipsychotics are generally more likely to induce extrapyramidal side-effects, but there are concerns over the safety of the atypicals in this age group (Reference Herrmann and LanctotHerrmann & Lanctot, 2006). The use of minimal effective doses seems vital here (as elsewhere in medicine).
Role of psychotherapy in treatment
Some expressions of troublesome personality traits will resolve with treatment of an associated or underlying functional disorder. However, when a patient has persistent or residual symptoms of personality disorder, a consistent approach from an experienced therapist may be of benefit.
As with younger patients with personality disorder, forming a therapeutic alliance can be difficult. Supportive, dynamic and cognitive approaches may be applicable, depending on the presenting complaint. It is important to have a consistent approach, with firm boundaries and good communication between the professionals involved. It is also important to involve the carers and to modify (if appropriate and possible) their reactions to untoward behaviour (Reference DavisonDavison, 2002).
Research suggests that the current generation of older adults are positively inclined to believe that talking therapy can help most people with depression and that they prefer psychological therapies to medication (Reference Rokke and ScoginRokke & Scogin, 1995). So, although older people may be initially less inclined to discuss their psychological issues, they appear not to be resistant to the idea of psychological intervention.
Nevertheless, the application of the psychotherapies has been slow to develop for this population, mainly because of ageism, negative stereotypes about the treatability of older people and a perceived lack of psychotherapeutic theories for later life (Reference HeppleHepple, 2004). The predominance of organic or biological models of old age may have biased the field towards ‘brain-based’ rather than ‘psyche-based’ explanations for illnesses in old age.
Cognitive–behavioural therapy
There is some evidence to suggest that adapted cognitive–behavioural therapy (CBT) is effective in addressing negative thoughts, identifying the dysfunctional cycles that can arise and intervening in unhelpful thinking patterns of older people (Reference Thompson, Gallagher and BreckenridgeThompson et al, 1987). In a recent article in this journal on the use of CBT with older people, Reference EvansEvans (2007) suggested how it might be modified to accommodate the degree of cognitive change and sensory and physical impairment encountered among such patients. Reference Barrowclough, King and ColvilleBarrowclough et al (2001) demonstrated the effectiveness of CBT v. supportive counselling for anxiety symptoms.
In old age, people often face great challenges related to disability and loss – their social roles diminish and vanish, partners and friends die. These can precipitate lowered self-esteem and depression. Again, antecedent cluster C personality traits might constitute predisposing factors.
Cognitive analytic therapy
Cognitive analytic therapy (CAT) may help patients to acknowledge some of these issues and work on them:
‘Personality and relationships are not adequately described in terms of objects, conflicts or assumptions. They are sustained through an ongoing conversation within ourselves and with others – a conversation with roots in the past and pointing to the future. In their conversation with their patients, psychotherapists become important participants in this conversation and CAT, I believe, fosters the particular skills needed to find the words and other signs that patients need’ (Reference RyleRyle, 2000).
Cognitive analytic therapy has been applied to late-life problems of patients with narcissism, borderline personality traits and post-traumatic syndromes (Reference Hepple and SuttonHepple & Sutton, 2004).
Psychodynamic therapy
Psychodynamic therapy is at least as effective as CBT in dealing with depression in older people (Reference Thompson, Gallagher and BreckenridgeThompson et al, 1987) but the patient's age can affect the nature of the transference and countertransference. In most cases, one might anticipate that the patient will be older – perhaps by a great deal – than the therapist, and this may be worth considering at the outset, during patient allocation and supervision.
Dialectical behavioural therapy
Older people with personality disorder who become depressed have been shown to be less responsive to depression-specific therapies (Reference RobinsRobins, 2003). In such cases, it appears that dialectical behavioural therapy may show promise (Reference LynchLynch, 2000). An adaptation of behavioural therapy, dialectical behavioural therapy aims to promote change in emotional ‘dysregulation’ (Reference RobinsRobins, 2003). Lynch found that it reduced interpersonal stress, hopelessness, avoidant, detached and emotional coping strategies, and also reduced dependency on, and desire to please, others.
Supportive psychotherapy
Supportive psychotherapy may be helpful for individuals with personality disorders who manifest low self-esteem and low self-confidence; it may also assist them in problem-solving and reducing the risk of future relapses or deterioration (Reference Bloch and BlochBloch, 1979). Psychodynamically oriented supportive therapy may help people to strengthen their ‘ego function’ and promote a better adaptation to reality (Reference RocklandRockland, 1989). Personality changes often occur in dementia, and supportive psychotherapy may help affected patients and also provide some support for their carers (Reference Junaid and HegdeJunaid & Hegde, 2007).
Family therapy
Likewise, family therapy may assist the families of people with dementia accompanied by personality change; it may be especially useful when counselling relatives before the diagnosis is revealed (Reference QuallsQualls, 2000). It can also inform awareness of family dynamics that are affecting the patient (Reference HeppleHepple, 2004).
Nidotherapy
Among younger people, there is growing evidence that nidotherapy may help to achieve a better fit, within the community, for people with personality disorders. It comprises a systematic adjustment of the environment to suit the needs of the individual (Reference Tyrer and BajajTyrer & Bajaj, 2005). The principles of nidotherapy might be applied to an older population to facilitate better coping skills and social functioning by manipulating their physical and social environment. The most obvious way of doing this is to offer patients access to residential care.
Conclusions
The literature concerning personality disorder among older people is currently quite sparse. This might be because personality disorders themselves have been rather contentious and, traditionally, old age psychiatry services have tended to focus on the management of dementia and the major Axis I disorders. However, it is likely that a greater number of patients with persistent Axis II disorders will survive into old age. Now would be a good time for psychiatric researchers to investigate the complex needs and issues associated with ageing among this group of people.
Declaration of interest
None.
MCQs
-
1 The following statements are correct:
-
a as age advances, impulsivity, aggression and promiscuity decrease
-
b among older people, antisocial and borderline personality traits become more common
-
c cluster A personality disorders are most prevalent among older people
-
d dementing illnesses always precipitate changes in personality
-
e among older people, trial of medication is always of help for personality disorder.
-
-
2 The following are very commonly associated with personality disorders in older people:
-
a depression
-
b metachromatic leukodystrophy
-
c anorexia nervosa
-
d schizophrenia
-
e autism.
-
-
3 When managing personality disorders in older adults:
-
a medications may not be useful in treating comorbid functional illnesses
-
b low-dose antipsychotics may help control disturbed behaviour
-
c older people believe that psychotherapy will not be useful for them
-
d psychotherapies have not been very useful
-
e ECT is a first-line treatment.
-
-
4 The following therapies have shown benefits in the treatment of personality disorder in later life:
-
a parenting therapy
-
b cognitive analytic therapy
-
c counselling
-
d homoeopathy
-
e aromatherapy.
-
-
5 The following ‘rules of thumb’ can be helpful in treating personality disorder:
-
a treat associated Axis I disorders
-
b support the patient only – exclude the carer(s)
-
c always try medication
-
d never use a psychotherapy
-
e never investigate underlying physical illnesses.
-
MCQ answers

| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | T | a | T | a | F | a | F | a | T |
| b | F | b | F | b | T | b | T | b | F |
| c | F | c | F | c | F | c | F | c | F |
| d | F | d | F | d | F | d | F | d | F |
| e | F | e | F | e | F | e | F | e | F |





eLetters
No eLetters have been published for this article.