Delusions are a key symptom of schizophrenia, occurring in about three-quarters of those diagnosed (Reference Sartorius, Jablensky and KortenSartorius 1986). They are frequently distressing and disabling and existing treatments are only partially effective. Many patients with schizophrenia show a relatively poor response to antipsychotic medication (Reference Lieberman, Stroup and McEvoyLieberman 2005; Reference Jones, Barnes and DaviesJones 2006), with about 50% of patients demonstrating persistent delusions even after the first acute psychotic episode has abated (Reference Craig, Garety and PowerCraig 2004). Research indicates that the effects of antipsychotic medication on delusional conviction in particular are less marked than on other aspects of delusions, such as associated distress and behavioural response (Reference Mizrahi, Kiang and MamoMizrahi 2006). Cognitive–behavioural therapy (CBT) for psychosis was initially developed to improve the treatment of persistent distressing delusions and hallucinations, and meta-analyses consistently indicate that this new intervention shows efficacy, but that the effects are small to moderate (Reference Pilling, Bebbington and KuipersPilling 2002; Reference Zimmermann, Favrod and TrieuZimmermann 2005; Reference Wykes, Steel and EverittWykes 2008). Although antipsychotic medication and CBT therefore both have benefits, research conducted worldwide demonstrates that the goal of delivering sustained improvement in delusions remains. Better treatments are needed, based on a sound understanding of cause and maintenance.
Cognitive theories of delusions
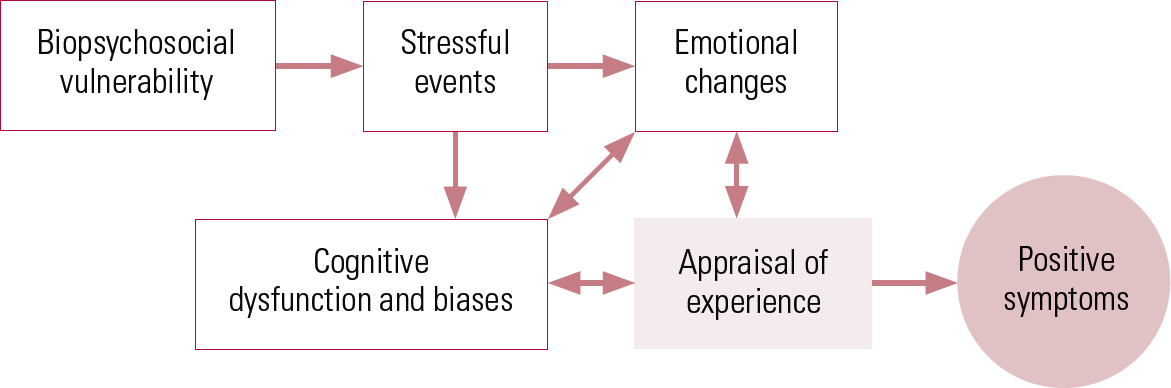
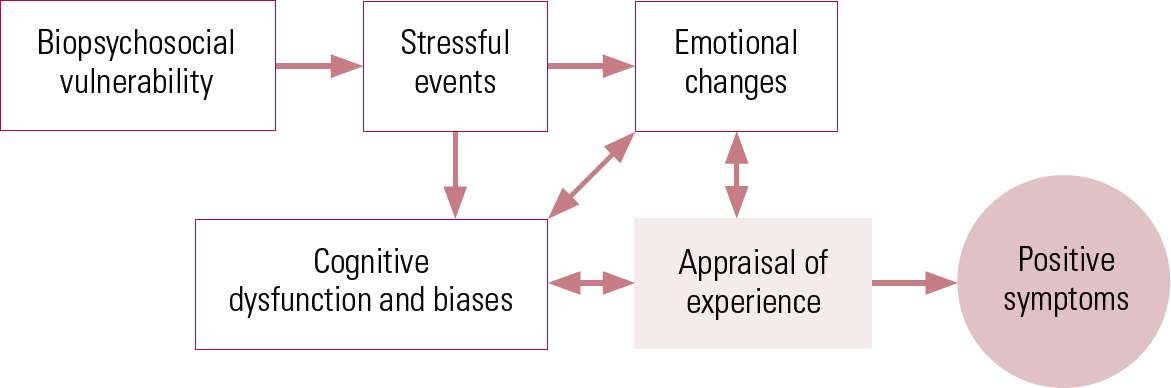
Over the past 10 years, the positive symptoms of psychosis, especially delusions, have become a focus of empirical research and are considered to result from a number of interacting biological, psychological and social factors (Reference FowlerFowler 2000; Reference Garety, Kuipers and FowlerGarety 2001; Reference Freeman, Garety and KuipersFreeman 2002; Reference KapurKapur 2003; Reference Van der GaagVan der Gaag 2006; Reference Garety, Bebbington and FowlerGarety 2007). Psychosis is considered to be complex and multifactorial. In a model first published in 2001, we adopted the widely accepted proposal that a person who develops psychosis has a premorbid vulnerability of biopsychosocial origin (in some combination of genetic, neurodevelopmental and psychosocial risks) (Reference Garety, Kuipers and FowlerGarety 2001; Reference Garety, Bebbington and Fowler2007).
Anomalous experiences in vulnerable individuals
In vulnerable individuals, stress triggers particular emotional and cognitive changes, resulting in anomalies of conscious experience such as hallucinatory voices. These anomalous experiences have been linked to information-processing and neurobiological disturbances (e.g. Reference KapurKapur 2003). We further proposed that specific reasoning and information-processing biases, pre-existing schematic beliefs about the self and others, current emotional disturbance and social factors (such as isolation and adversity) both singly and in combination lead vulnerable individuals to appraise the origins of these anomalous mental states as external. As a result, the abnormal beliefs and hallucinations become symptomatic. Thus, the experience, for example, of a voice does not necessarily develop into a full-blown psychotic symptom.
Anomalous experiences and a ‘need for care’
Many people in the general population experience voices and other psychotic experiences at certain stages of their lives, without developing a ‘need for care’ (Reference van Os, Hanssen and Bijlvan Os 2000; Reference van Os, Hanssen and Bijl2001), which only occurs when an individual appraises the experience in particular ways – such as that it comes from an external source and is personally significant and uncontrollable. It is the particular interpretation or appraisal that causes the associated distress and disability, rather than the experience itself. This emphasis on the role of appraisal is in common with cognitive models of other disorders, such as Beck et al ’s cognitive model of depression (Reference Beck, Rush and Shaw1979). A cognitive model of psychosis is represented schematically in Fig. 1.
There are thus three central propositions of cognitive models of psychosis that concern delusions and reasoning (Box 1):
-
• psychotic experiences in themselves are not pathological; they are present in a substantial minority of the general population (5–30%) without necessitating a need for care;
-
• it is the appraisal of these experiences that is central to the development of pathological symptoms; and

FIG 1 A cognitive model of the positive symptoms of psychosis (Reference Garety, Kuipers and FowlerGarety 2001).
-
• based on experimental evidence, a number of cognitive and emotional processes are hypothesised to contribute to this biased appraisal, one of which is reasoning biases (for reviews of the literature see Reference Garety, Kuipers and FowlerGarety 2001, Reference Garety, Bebbington and Fowler2007).
BOX 1 Three key propositions of cognitive models of delusions
-
1 Psychotic experiences such as voices are not in themselves pathological
-
2 The appraisal of psychotic experiences is central to the development of symptoms
-
3 Reasoning biases influence appraisals and so are risk factors for delusions
Delusions and reasoning biases: data-gathering (jumping to conclusions)
Cognitive models thus propose that processes which contribute to biased appraisals are risk factors for the development of delusions. One factor that has been highlighted is reasoning biases. Delusions have been shown with particular consistency to be associated with reduced data-gathering: this has been repeatedly demonstrated using probabilistic reasoning tasks based on a Bayesian model of probabilistic inference (Reference Garety and FreemanGarety 1999; Reference Fine, Gardner and CraigieFine 2007; Reference FreemanFreeman 2007).

FIG 2 The Beads Task as seen on-screen. Pink represents the orange viewed by participants.
The Beads Task
In a typical probabilistic reasoning task (the Beads Task; Fig. 2), participants are asked to request as many pieces of evidence (coloured beads) as they would like before deciding from which of two hidden jars the beads are drawn. The participants are shown that the jars have beads of two different colours and are informed of the proportions of each coloured bead in the jars. In the original version of the task, one jar has 85 black beads and 15 orange beads and the other jar has the opposite ratio of beads. In a more difficult version the beads are in the ratio 60:40. The key variable employed is the number of items requested before making a decision. Individuals with delusions request fewer beads before making their decision than psychiatric or non-clinical controls.
In a review of studies employing this paradigm, all ten studies that compared a group with delusions with a non-clinical control group found significant differences in numbers of beads drawn. The extreme form of the bias – ‘jumping to conclusions’ (JTC) – has been operationalised as when a decision is made after two or fewer beads. About 50–70% of people with delusions jump to conclusions when the beads are in the ratio of 85:15, compared with about 10% of non-clinical controls (Reference FreemanFreeman 2007); around 40% of people with delusions jump to conclusions even when the beads are in the difficult ratio of 60:40 (Reference Garety, Freeman and JolleyGarety 2005).
The JTC bias has been replicated widely, using various modifications of the basic paradigm, not only in people with delusions, but also in people who have recovered from delusions, people at risk of delusions and people with delusion proneness in the general population (Reference Fine, Gardner and CraigieFine 2007; Reference FreemanFreeman 2007; Reference Moritz and WoodwardMoritz 2007a). That the bias is present in at-risk populations and in remitted groups, although in an attenuated form, suggests that it is a trait representing liability to delusions, but that it may in addition be exacerbated in acute delusional states (Box 2). Taken together, this research indicates that this bias is a trait that may contribute to both delusion formation and persistence. The evidence also shows that this is a data-gathering bias rather than a deficit in probabilistic reasoning. The reasoning bias is specifically associated with levels of delusional conviction.
BOX 2 Key facts about jumping to conclusions
-
1 Reduced data-gathering on the ‘beads’ task is consistently associated with delusions
-
2 An extreme jumping-to-conclusions bias is present in 40–70% of currently deluded people
-
3 Reduced data-gathering also occurs in at-risk and remitted groups, suggesting that it is a trait representing liability to delusions
What is jumping to conclusions? Possible mechanisms for the bias
We know that JTC involves reduced data-gathering and making decisions under conditions of uncertainty on the basis of little evidence (Box 3), but the mechanism for this bias is not yet clear, and a wide variety of proposals have been made. Some hypotheses involve impulsivity or emotional processes, such as anxiety, whereas others invoke neurocognitive deficits (Reference Fine, Gardner and CraigieFine 2007; Reference Ross, Freeman and DunnRoss 2009).
BOX 3 Personal account
‘As the months went by, my mind was getting riskier and riskier in decision making style. [In time] I was actually walking past people listening almost masochistically for “comments at my expense”. Every “him” or “he” was now a hit… A woman in a main street took a long, very hard look at my face as she was walking towards me, ran ahead, with urgency, to catch up her partner and said loudly, “Hey”. I didn’t hear the rest of what she said but it must have been about me.’
(Reference Chadwick, Freeman, Bentall and GaretyChadwick 2008)
Anxiety
There is little evidence to suggest that impulsivity accounts for JTC, since, for example, it is not related to faster responding on the task and people who show the JTC bias do adjust their behaviour appropriately when probabilities are changed. There is, however, evidence to suggest that JTC may be exacerbated by anxiety, both when anxiety is experimentally manipulated (Reference Lincoln, Lange and BurauLincoln 2009) and under conditions of exposure to an everyday setting that provokes increased anxiety (the Camberwell Walk study; Reference Ellett, Freeman and GaretyEllett 2008). Another experimental study, however, did not replicate the effect of anxiety on JTC (Reference So, Freeman and GaretySo 2008). The jury is thus still out on this question. But, clearly, if anxiety is a factor in inducing or exacerbating JTC, this may suggest particular interventions.
Neurocognition
The evidence with respect to neurocognition is also quite limited. Reference Broome, Johns and ValliBroome et al (2007) found an association of JTC with impaired working memory. Reference Bentall, Rowse and ShryaneBentall et al (2009), using structural equation modelling, found that JTC appeared to be related to paranoia via a cognitive functioning factor, which partially comprised tests that they considered to reflect executive functioning, including a test of working memory (backwards digit span). There is therefore some emerging evidence of a link with working memory. However, associations between JTC and working memory or other cognitive impairments have not been consistently shown. The relationship of JTC to the well-attested cognitive impairments of schizophrenia (such as attention, memory and executive function deficits) is only just starting to be examined systematically (e.g. Reference Woodward, Mizrahi and MenonWoodward 2008; Reference van Hooren, Versmissen and Janssenvan Hooren 2008), with inconclusive results.
It should be noted that JTC differs from these cognitive impairments in schizophrenia in that, unlike them, it has been shown to be specifically related to delusional symptoms. The mechanism for JTC may therefore involve working memory, but at present it remains an open question.
Belief flexibility
Many people with delusions produce few alternative explanations for the evidence cited for their beliefs, do not think that they could be mistaken in their belief and report that they would not change their belief in a hypothetical contradiction task. These findings have been incorporated into the concept of belief flexibility (Reference Ross, Freeman and DunnRoss 2009). Belief flexibility refers to ‘a meta-cognitive process about thinking about one’s own … beliefs, changing them in the light of reflection and evidence and generating and considering alternatives (Reference Garety, Freeman and JolleyGarety 2005, p. 374). Reference Colbert, Peters and GaretyColbert and colleagues (2010) have shown that whereas belief inflexibility is characteristic of all strongly held beliefs, whether delusions or strongly held beliefs in the general population, people with delusions were more inflexible than controls about standard non-delusional beliefs, suggesting people with delusions may have a more general propensity to inflexibility. There have been indications that belief flexibility predicts a positive response to both antipsychotic medication and CBT. Belief flexibility is strongly related to JTC (Box 4). We found evidence that belief inflexibility mediates the effect of JTC on delusional conviction. We have proposed that JTC limits belief flexibility, thereby maintaining and escalating levels of delusional conviction (Fig. 3).
BOX 4 What is the JTC bias?
Jumping to conclusions (JTC):
-
• is a data-gathering bias leading to decisions based on little evidence
-
• may be exacerbated by anxiety
-
• may be related to impairments in working memory
-
• is related to limited belief flexibility
JTC and response to treatment
In a novel line of research, it has been shown that JTC may moderate the response to antipsychotic treatment in a drug-naive group of patients with a first episode of psychosis, such that those with an extreme JTC bias showed a poorer treatment response (Reference Menon, Mizrahi and KapurMenon 2008). The bias was not changed in this sample following administration of anti-psychotic medication. Jumping to conclusions also does not appear to change in response to standard CBT approaches (Reference Brakioulas, Langdon and SlossBrakioulas 2008; Reference Garety, Fowler and FreemanGarety 2008). Thus, on the current evidence, JTC is not changed by treatment but might moderate treatment effects, whether the treatment is psychological or pharmacological.
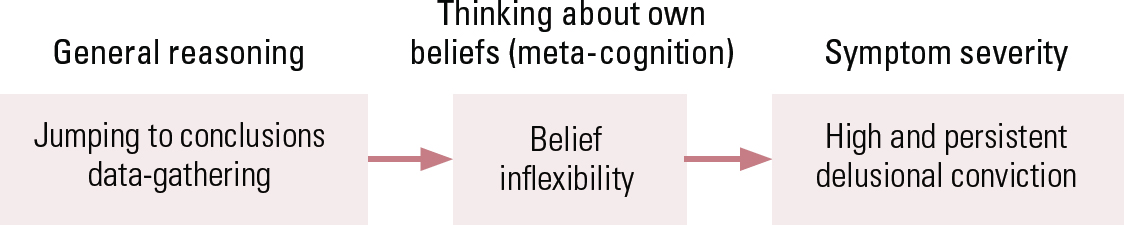
FIG 3 Reasoning processes in delusional conviction.
Thus, there is ample evidence that JTC is associated with delusions and further evidence that it is related to limited belief flexibility, that it is not typically changed by treatment, whether pharmacological or psychological, and that there are indications that it moderates treatment effects. We therefore conclude that JTC is a key target for treatment: novel strategies aimed at reducing JTC and improving data-gathering are likely to be beneficial in enhancing belief flexibility and thereby assisting reappraisal of delusional beliefs.
This research therefore points to a new strategy for treatment development. Cognitive–behavioural therapy is a psychological therapy that aims to assist with reappraisals of thoughts, emotions and experiences. However, thus far, the evidence suggests that CBT, as generally delivered, does not affect JTC. A more direct and intensive approach, targeting these key reasoning processes, might have therapeutic benefit and be incorporated into CBT. Furthermore, this is of theoretical importance. If changing reasoning style alters delusional ideation, this will support the claims of cognitive models that hypothesise that reasoning has a causal role in delusions.
Developing a new treatment approach for delusions: reasoning training
We have, therefore, embarked on a programme of treatment development, targeted at the JTC bias, to aim to improve the effectiveness of treatment for delusions. To date, only a small number of studies have aimed to manipulate the JTC bias. Reference Moritz and WoodwardMoritz and colleagues (2007a,Reference Moritz, Burlon and Woodwardb) report the development of a group-based ‘metacognitive training’ (MCT) package targeting a number of cognitive processes, which include JTC. Training is delivered over eight sessions, each lasting 45–60 minutes. In two small pilot studies (Reference Moritz and WoodwardMoritz 2007a; Reference Aghotor, Pfueller and MoritzAghotor 2010) the intervention was found to be well received by participants and appeared to be associated with a decline in both JTC and positive symptoms, although not all effects were statistically significant and further research is clearly warranted. In our first study (Reference Ross, Freeman and DunnRoss 2009), we sought to demonstrate, employing a brief computerised reasoning training, that it is possible to improve data-gathering (thus reducing JTC) in people with delusions. A secondary aim was to explore whether improvements in reasoning would lead to improvements in flexibility in thinking about delusions. It was also planned to examine whether metacognitive training reduced delusional conviction. However, since delusional beliefs are strongly and persistently held, it was considered unlikely that brief training would lead to significant and immediate reductions in delusion conviction.
A new reasoning training intervention – two studies
The original study
In the first study (Reference Ross, Freeman and DunnRoss 2009), we developed a computerised training program, designed to use engaging material of a neutral content. It aimed to convey the overall idea that it is preferable not to reach a decision too quickly. Participants were presented with three training tasks, each lasting 15 minutes, that illustrated the targeted reasoning biases and ways of correcting them. The program focused on data-gathering, generation and consideration of alternative ideas and the use of confirmatory and disconfirmatory evidence.
Object identification and picture interpretation
Two of the tasks (object identification and picture interpretation) were adapted from previously devised modules of the metacognitive training package, designed for group administration by Reference Moritz, Burlon and WoodwardMoritz and colleagues (2007b) and described in Moritz & Woodward (Reference Moritz and WoodwardMoritz 2007a).
Visual illusions
The third task, visual illusions, was designed specifically for this study. The whole training was presented using Microsoft PowerPoint during a 45-minute session. The content of training was not discussed in relation to the participants’ delusions or any aspect of the clinical assessment. This was because we wished to establish whether an intervention that solely targeted the reasoning process and not the content of delusions would have the hypothesised effects on data-gathering and belief flexibility. Each task had three phases: presentation of stimuli and free response; review of initial responses and instruction in reasoning; and further practice with additional stimuli. Further detailed descriptions of the training tasks are given in the report on our first study (Reference Ross, Freeman and DunnRoss 2009).
We recruited 34 people with a diagnosis of schizophrenia spectrum disorder and current delusions, held with at least 75% conviction. They were randomly allocated to the 45-minute reasoning training or to an attention-control condition (neuropsychological testing). The brief, single-session training intervention affected data-gathering, reflected in a significant increase in the number of beads requested on both versions of the beads task immediately after training. The study therefore demonstrates that it is possible in the short term to change the data-gathering pattern of people with delusions. Another finding was that JTC at baseline moderated the effects of training: those with an extreme JTC style benefited less from the training. As noted above, a prior JTC bias has been found to moderate change in response to antipsychotic medication (Reference Menon, Mizrahi and KapurMenon 2008). In this study, a prior JTC bias moderated the effects of reasoning training. It was clear that training improved data-gathering more among those individuals with delusions who did not show the JTC bias at the outset. This leads to the conclusion that JTC in people with delusions is a strong bias that is somewhat unresponsive to only a brief training intervention. There were also improvements in the training group on belief flexibility and delusional conviction, although these fell short of significance.
An enhanced study
The results of this first study were sufficiently encouraging to justify further development of this training approach. Our second study is now completed and it includes 13 participants with delusions assessed in detail, pre-and post-training and at 2-week follow-up (Reference Waller, Freeman and JolleyWaller 2011). The training intervention has been substantially developed (Box 5). It is more interactive and makes use of humour and multimedia, with film clips and commissioned video material. It emphasises reasoning processes, but, to attempt to have a greater impact and relevance, it incorporates socially ambiguous and delusion-relevant content.
BOX 5 Reasoning training modules
-
1 What’s the picture: data-gathering
-
2 Illusions: looking closely, inhibiting initial response
-
3 First impressions: data-gathering
-
4 Different explanations: generating alternatives
-
5 JTC in the movies: humorous clips consolidating learning
This newer training package has five modules, lasting about 3 hours in total. The first two modules are from our first study (Reference Ross, Freeman and DunnRoss 2009; one a modification of Reference Moritz, Burlon and WoodwardMoritz 2007b) and three are completely new. Task four, for example, was designed to introduce the idea of thinking about alternative explanations for events or situations before reaching a conclusion. Participants were given three scenarios, each with potential for a paranoid interpretation. For example, in scenario one, participants were asked to imagine that they are in a cafe and notice that someone seems to be pointing and staring in their direction. A short video clip illustrating each scenario was presented. After seeing each clip, participants were asked to think about possible explanations for each scenario and were prompted to think about neutral, positive and negative interpretations (e.g. ‘What might you think if you were feeling scared or worried?’). They were also given the option of seeing some ideas, already devised by the researcher (e.g. ‘They have mistaken you for someone else’; ‘They are angry with something you have done’).
During the training phase, participants were given the option to search for more evidence in the form of three further video clips. For example, in scenario one they were shown the original clip again, a close-up picture of the person, and finally a clip of the camera panning around to reveal a television showing sports behind them. Participants were then asked to pick which of their explanations seemed most likely. Finally, they were told how people might have jumped to conclusions in that situation, given the paranoid interpretation, and suggested that this could negatively affect their feelings and behaviour. If participants suggested very paranoid interpretations, this was gently pointed out by the researcher and it was suggested that thinking about possible neutral explanations could help them to see the situation differently and feel less threatened as a result.
This package includes paranoia and other delusion-relevant material, so we gathered feedback from participants as to its acceptability. Participants with delusions overwhelmingly reported that they found it acceptable and helpful (Box 6).
BOX 6 Participants’ experience of the training
-
• ‘The programme was easy to follow. It makes you think carefully about what you’re doing. I learnt to slow down to make judgements, looking closely at arguments, and not reacting immediately but gathering evidence’ (Participant A, post-training)
-
• ‘I noticed myself jumping to conclusions – I saw a woman walking around the housing estate. Under normal circumstances I would have found this really dodgy, but I asked a neighbour who’d been out gardening about her and she was looking for her lost cat. I felt a lot better then.’ (Participant B, at 2-week follow-up)
The training was more effective than in our first study (Reference Ross, Freeman and DunnRoss 2009), as intended. Post-training and at 2-week follow-up, we found significant and large effects on improving belief flexibility and reducing delusional conviction, and a small, non-significant effect on data-gathering (Reference Waller, Freeman and JolleyWaller 2011). Over half of the participants (62%) benefited. The training was also very well received by participants, with high ratings for interest in, and enjoyment and usefulness of, the program. This is a preliminary small-scale, uncontrolled study; the next step is to evaluate effects in a larger, controlled study, which is now underway.
Implications for clinical practice
The research described here also has some implications for clinical practice (Box 7). In our clinical practice, we are alert to the role of JTC in the thinking of people with delusions. We may discuss reasoning styles explicitly and normalise JTC –‘everyone jumps to conclusions sometimes’. We discuss and illustrate how this can lead to errors of judgement, using examples from everyday life or the media. (Much humour and many television advertisements rely on JTC for their impact.) We try to model an open and flexible style of thinking, expressing doubt and considering alternative viewpoints. We explore collaboratively the patient’s reasoning processes in specific situations, initially focusing on everyday situations and only gradually considering times when delusions have been prominent. Bearing in mind the suggestive findings on anxiety and working memory, we will discuss the potential role of anxiety or difficulties in holding all of the information available to make good decisions. We also plan ‘homework’ tasks involving improving decision-making about specific appraisals of experiences by gathering data and considering alternatives. Very direct work using cognitive therapy approaches on delusional beliefs, should, we consider, be undertaken with due care and in the context of an established therapeutic relationship and therapy. However, more general discussion of improving everyday reasoning should be broadly helpful and can be undertaken in a range of therapeutic consultations.
BOX 7 Clinical implications
-
1 Be alert to the role of JTC in delusions
-
2 Model an open and flexible style of reasoning in consultations with patients
-
3 Examine how JTC leads to errors of judgement in everyday life and normalise JTC
-
4 Discuss how to improve everyday decision-making
Conclusions
We have presented in this article findings about reasoning biases in delusions leading to a new approach to treatment. From our cognitive model, we identified a key, theoretically derived and empirically validated process, the JTC reasoning bias. We have developed a targeted intervention for this bias and evaluated it in pilot studies. The results of these studies are fully consistent with the hypothesis that JTC reasoning bias has a causal role in delusional conviction by influencing appraisals, as proposed by the cognitive model. We consider that the intervention has the potential to improve outcomes for people with delusions. If positive effects are confirmed, we plan to incorporate and test the intervention as one component of a personalised CBT for delusions, and in combination with a trial of antipsychotic medication.
MCQs
Select the single best option for each question stem
-
1 The proportion of people with delusions in whom jumping to conclusions (JTC) occurs is about:
-
a 5%
-
b 10%
-
c 50%
-
d 95%
-
e 100%.
-
-
2 JTC is deemed to be present when decisions in the 85:15 beads task are made after the following number of beads:
-
a 0
-
b 2 or fewer
-
c 5 or fewer
-
d 8 or fewer
-
e 10 or fewer.
-
-
3 It has been shown to be possible to change JTC using:
-
a intensive reasoning training approaches
-
b antipsychotic medication
-
c standard cognitive–behavioural therapy
-
d in-patient admission
-
e out-patient consultations.
-
-
4 JTC has not been found to be associated with:
-
a anxiety
-
b working memory
-
c belief flexibility
-
d impulsivity
-
e executive functioning.
-
MCQ answers

| 1 | c | 2 | b | 3 | a | 4 | d |







eLetters
No eLetters have been published for this article.