The epidemiology and management of schizophrenia have been well studied over the past few decades. In the UK, key findings that have emerged time and again are the excess prevalence and incidence rates of schizophrenia among people of African–Caribbean origin. The reasons for this excess and the implications of this finding are many. The findings may reflect a true excess or a methodological artefact related to errors in the estimation of numerator and denominator data. The findings have been increasingly accepted as better designed studies have emerged, but these still do not fully address concerns about the nature of schizophrenia in other cultural groups and in societies in which industrialisation and economic productivity of the individual are not considered to be as crucial for an individual's sense of belonging in a community.
Other implications include individual and family distress related to the loss of hopes and expectations and being seen as a high-risk group for a condition that carries stigma. In addition, there is economic burden on the individual, family and society if unemployment and disability diminish financial security. There are also significant implications for service providers and planners, who are required to meet the health and social care needs of sufferer, family and community in order to maximise the chances of a functional recovery at each of these levels.
Problems in studying rates
There are several problems in studying rates of schizophrenia in any ethnic group. First, the heterogeneity of ethnic groups and limitations of ethnic group definitions are not fully appreciated, but they must be understood for meaningful interpretation of prevalence and incidence studies. Second, the definition of schizophrenia has been criticised for adopting a disease model and for universal application of a Western concept that may not have validity as an illness, disease or disability in other societies. The existence of schizophrenia is deduced on the basis of clinical diagnostic practice, which varies within and across cultures, societies and economic systems. For example, the syndrome of sluggish schizophrenia in the former USSR demonstrated how diagnostic criteria are permeable to value judgements that promote a society's moral and political ideology. Diagnostic formulation may also emphasise as pathological symptoms phenomena that are prominent in non-schizophrenic psychoses and in culturally sanctioned states of distress.
Thus, studies generally have looked at incidence cases of a syndromal diagnosis without attention to local contexts, and this leads to the interpretation of data in isolation from cultural, social and historical biographies. Depending on the position one takes – universalist or relativist, not to mention psychiatrist as physician or psychiatrist as shaper of social conditions – these data will be interpreted in markedly different ways. Although methodological and interpretative flaws in studies have received increasing attention as the data have been gathered, they are often defined from within the same closed system of thinking. Cross-fertilisation between different systems of research methods is rarely witnessed, but is necessary for a more global interpretation of the data, rather than a psychiatric and purely medical research-oriented interpretation that is founded on assumptions that are not easy to question from within the closed system. Therefore, a fuller and more complete appreciation of the true position requires that one interpret the data with and without these assumptions. In this paper, however, we assume the research data to reflect a truly higher incidence and prevalence of schizophrenia. We consider the possible explanations for these findings with an emphasis on sociocultural perspectives.
In the literature, terms used to describe the group of African–Caribbeans have included ‘Afro-Caribbeans’, ‘Blacks’ and ‘Negros’. Such etymological use illustrates difficulties in identifying both the denominator and the numerator in ascertaining rates of illness. In this paper, we first present American studies on samples that are now identified as African–Americans; then we present UK studies on people commonly identified as African–Caribbeans. We compare the two groups, drawing out similarities and differences.
American studies
American studies have not specifically identified Caribbean populations, although these might have been included in their data. Hence, direct comparisons between the studies in the USA and the UK are not valid. In 1850, rates of mental illness among the ‘Negro’ cohort were 17.5 per 100 000 population, but had shot up to 91.2 per 100 000 within 30 years (Reference BabcockBabcock, 1895). The increase in rate was attributed by Babcock to emancipation of the slaves: slaves did not get excited because they did not indulge in political discussions, did not participate in religious activities and did not have any anxieties. It is possible that some of the increase was indeed the result of the release of slaves with mental illnesses, who then ended up in asylums, whereas previously they may have been dealt with on the plantations. Green (1914) reported that the 6:1 ratio of White v. Black admissions on his unit changed to 1:4 between 1870 and 1880 and over the next year to 1:2.2. Drugs and toxic psychosis were said to be more common in Whites, whereas Blacks had higher levels of senile psychosis, general paralysis, dementia praecox and manic–depressive psychosis. Chasson (1963), reporting on first admissions to a psychiatric hospital in Washington DC between 1950 and 1957, showed that White males were more likely to be discharged compared with White females, who in turn were more likely to be discharged compared with Black males. Black females had the lowest discharge rates. Discharge from hospital depended upon a number of factors. However, Chasson (1963) argued that the hardships endured by Blacks intensified the psychopathology. Crawford et al (1960) set out to test whether the rates of mental illness differed between Blacks and Whites, using ethnically matched interviewers. The rates based on known cases were similar in both groups. The Black samples saw mental illness as a problem that people brought on themselves. The authors postulated that, because Blacks lived in a minority culture, when problems became extremely difficult to control they ‘invited’ dominant White authorities to intercede.
Data for differential rates of mental illness among Blacks and Whites were mixed (as shown in Table 1). The variation has been attributed to confusion between prevalence and incidence and definitions of schizophrenia. Jaco (1960) was the only author to show that rates of psychosis were highest in Anglo-Americans, followed by non-Whites and fianally Spanish–Americans, who had the lowest rates. Marital status was shown to be an important factor. Snowden & Cheung (1990) reported that for all types of in-patient care schizophrenia was diagnosed consistently more often for Blacks (56.3%) than for Whites (31.5%). Some authors (e.g. Mukherjee et al, 1983) have suggested that auditory hallucinations are subject to pathoplastic cultural influences and may therefore be interpreted wrongly, undue emphasis being given to pathological explanations leading to misdiagnosis (see Racism below). Misdiagnosis has indeed become a more important issue, of which patients, carers and some mental health professionals complain. Misdiagnosis can arise from ignorance of the cultural variability in expressions of distress, or where psychopathological phenomena have differing significance across cultures, or where cross-cultural stereotyping (by patient and doctor) leads to difficulties in obtaining a sufficiently detailed history. However, misdiagnosis alone cannot explain all the findings in both the USA and the UK. Although misdiagnosis is assumed to mean overdiagnosis, interpreting the behaviour of Black adolescents from low socio-economic urban dwellings as normative has also led to professionals missing or ignoring underlying psychiatric disorders. This also constitutes a form of institutional practice that leads to poorer outcomes for Black people. In any assessments the clinician must be aware of some basic principles (see Box 1).
Box 1. Good practice points in assessing a case of schizophrenia
Take a careful history
Understand delusional phenomena in cultural context
Understand hallucinatory experience in cultural context
Check thought disorder in primary language
Ascertain abnormal mood states
Ascertain passivity phenomena
Carry out a physical and neurological examination
Carry out physical investigations
Check third-party information, including cultural identity¤
UK studies
Since the late 1960s, a number of studies have been carried out in the UK. Apart from the above-mentioned problems of incidence and prevalence, these authors often relied on denominators that were not entirely accurate because under-enumeration in census data was particularly prevalent among Black and ethnic minority groups. We have divided these studies into two periods – before and after 1980 – largely because more epidemiologically sound studies were carried out after the 1980s.
Before 1980
Hemsi (1967) used Camberwell case-register data and reported that the rates of case-note diagnosis of schizophrenia were 4.5 times higher in African–Caribbeans. Organic psychosis, alcoholism and drug dependence were absent in the African–Caribbean population. Kiev (1965) found higher prevalence rates of mental illness among Blacks attending a general practitioner (GP) surgery in south London compared with Whites. Both these studies focused on GP attenders. Rwegellera (1977) too used the Camberwell case register, but over a 3-year period, and calculated that inception rates of schizophrenia were 0.92 per 1000 among West Indians compared with 0.12 per 1000 among Whites and 4.18 per 1000 among West Africans. Using age-standardised data, for 15- to 24-year-olds, West Indian rates were 1.40 per 1000 compared with 0.16 per 1000 for Whites; for 25- to 44-year-olds, these rates were 0.80 per 1000 and 0.17 per 1000 respectively for the two groups. Ethnicity was determined using country of birth. Small numbers of base population and the use of admissions case-note data provided indicators at psychiatric service contact level only, rather than a population-based picture in which help-seekers and only help-seekers would be included.
After 1980
Carpenter & Brockington (1980) found from hospital case notes in Manchester that rates of schizophrenia among West Indians were five times higher than those among Whites. Dean et al (1981), in south London, reported that rates of schizophrenia were five times higher in African–Caribbeans compared with their White counterparts (see Table 2).
Littlewood & Lipsedge (1981) interviewed 36 patients who had presented to the hospital with symptoms of a religious fervour. Of these, 20 were African–Caribbeans, four West Africans and eight White. Among the first two groups, 70% of the sample were female. The symptoms were of gross excitement, violence and hostile irritability. There was no doubt about the diagnosis of psychosis, but doubt existed about its exact type.
Harrison et al (1988), using the rigid criteria previously used for World Health Organization studies over 2 years, collected cases of first onset of schizophrenia and observed that mean annual incidence among African–Caribbeans aged 15–54 years was 13.5 per 100 000, 10 times that reported in the White population. Mean annual rates for ages 16–29 years was 36.4 per 100 000, 18 times the rate in general populations. A key problem remained in calculations of the denominator; also, they compared their data with White populations for whom the sample had been collected a few years previously.
McGovern & Cope (1987) collected data from case notes of admissions to a Birmingham hospital and found that first admission rates for 16- to 29-year-olds were 53.8 per 1000 for Whites, 360.2 per 1000 for African–Caribbean migrants and 246.0 per 1000 for African–Caribbeans born in the UK. The rates among females of the two groups were broadly similar. Harvey et al (1990) reported that, for 15- to 24-year-olds, admission rates in south London were 186 per 100 000 for all African–Caribbeans (both migrant and UK-born) compared with 58 per 100 000 for Whites. Three-quarters of African–Caribbean patients were unemployed compared with just over half (56%) of Whites. The relative risk was slightly lower for their older sample.
In the early 1990s, a spate of prospective studies were set up. King et al (1994), in north London, reported that rates of schizophrenia were 1.2 per 10 000 for Whites, 4.6 per 10 000 for Black groups (5.3 for Black Caribbeans) and 15.3 per 10 000 for Pakistanis. The latter group had only two patients, as did some other groups, making generalisation a problem. Bhugra et al (1997), over a 2-year period, collected cases of psychosis among African–Caribbeans, Asians and Whites over 1 year in the same geographical area and reported that rates for Whites were 3.0 per 10 000 compared with 3.6 per 10 000 for Asians and 5.9 per 10 000 for African–Caribbeans. When age-standardised for 18- to 29-year-olds, these rates were 14.7 per 10 000 for African–Caribbeans and 7.5 per 10 000 for Whites. The African–Caribbean group had more males, and rates of unemployment were 82% compared with 22% in the general population and 55% among Whites. One-third of African–Caribbeans were living alone and logistic modelling showed that ethnicity, age and gender were key factors in association with schizophrenia.
Harrison et al (1997), in another prospective study from Nottingham, reported that the standardised incidence rate (SIR) for all psychotic disorders was higher in the African–Caribbean groups. For schizophrenia, the age-standardised rate ratio between the African–Caribbean and the White sample was 8.1, with SIRs of 46.7 per 100 000 and 5.7 per 100 000 for the two groups respectively. A vast majority of African–Caribbeans (81%) were born in the UK and the rest in the Caribbean, suggesting that those African–Caribbeans who are born in this country still have considerably higher rates. In one of the few community-based prevalence studies, Nazroo (1997) observed that annual prevalence of non-affective psychotic disorders was higher for African–Caribbeans, compared with Whites (13 per 1000 v. 8 per 1000).
From our review, some common themes start to emerge, the first being that, bearing in mind the caveats discussed above, incidence rates of schizophrenia are consistently higher among the African–Caribbeans, especially the younger age groups. The aetiological factors of schizophrenia are many and it would appear that ethnicity alone may not be able to explain such a variation.
Hypotheses for high rates
Many explanations for differential incidence rates of schizophrenia have been hypothesised (see Box 2). Discussion of these hypotheses has to be seen in the context of heterogeneity of the African–Caribbean samples. Using the Mental Health Enquiry data for admission and ethnicity, Glover (1989) was able to demonstrate that annual rates of admissions over a 3-year period were highest among Jamaicans (6.82 per 1000 for men and 6.33 per 1000 for women) compared with 4.19 per 1000 for men and 4.47 per 1000 for women among those born in Barbados and 3.61 per 1000 for men and 4.08 per 1000 women born in Trinidad and Tobago. However, for schizophrenia, Jamaican men and Barbados-born men had similar rates and Trinidad-born were the lowest, whereas for mania, Trinidad-born men had the highest rates. This is a rare study that makes a distinction between different Caribbean islands, thus showing the importance of defining the cultural groups with some precision. The severity of economic conditions in the Caribbean, as in other countries, is a key factor in genesis of ill health. Bearing in mind this heterogeneity of population, the problems of data collection and diagnosis and the varying socio-economic factors, the following hypotheses for explaining high rates are put forward.
Box 2. Hypotheses for high rates
Genetic factors
Pregnancy and birth complications
Social factors:
-
• Social inequality
-
• Economic factors
-
• Discriminations
Racism:
-
• Harassment
-
• Racial life events
Population density
Genetic factors
The rates of strictly and narrowly defined schizophrenia are reasonably uniform across different cultures and different nations, whereas rates of broad-definition schizophrenia vary. Studies have shown that among White populations genetic factors contribute to the risk of schizophrenia. If the increased incidence of schizophrenia among UK-resident African–Caribbeans were owing to a special genetic vulnerability (for example, an inherited polymorphism) that showed linkage to genes coding for physical (racial) appearance, and this conferred a greater risk among African–Caribbeans than exists among Whites in the UK, we would expect similar and higher incidence rates in all African–Caribbean populations. Incidence rates among African–Caribbeans in Jamaica are the same as those among Whites in the UK. The incidence rate among British-born African–Caribbeans is higher than among Caribbean-born African–Caribbean peoples. The lifetime risk of schizophrenia increases ten-fold among siblings of an affected individual and is almost 50% for identical twins. Sugarman & Crauford (1994) reported that siblings of patients with schizophrenia in the African–Caribbean groups were at significantly higher risk than any other group of relatives. These findings were replicated by Hutchinson et al (1996), who found that siblings of second-generation schizophrenia probands had a morbid risk of schizophrenia four times higher than that of their White counterparts. The overall conclusion is that the excess incidence of schizophrenia among African–Caribbean people cannot be explained by genetic vulnerability alone. McKenzie et al (1995) found that UK-resident African–Caribbean people with schizophrenia had a better prognosis and suggested this finding to be more compatible with psychosocial and environmental risk factors rather than genetic aetiology.
Pregnancy and birth complications
Some researchers have shown that pregnancy and birth complications (PBCs) are associated with schizophrenia (Reference McGrath, Murray, Hirsch and WeinbergerMcGrath & Murray, 1995), although this has been challenged (Reference Kendell, McInneny and JuszczackKendell et al, 2000). We have observed that, in Trinidad, with normal rates of schizophrenia, PBCs were actually lower than those reported for the African–Caribbean populations in the UK. With such a limited number of studies, this causative factor cannot be ruled out entirely, but certainly such observations, if replicated in Jamaican and Barbadian samples, will rule out PBCs as a possible causation in this group. Related to PBCs are other neurodevelopmental delays and factors, which have not been studied in the African–Caribbean group.
Social factors
The effects of social environment and social factors such as life events in the genesis and outcome of schizophrenia are well known. The differences between migrants and their children may well be related to a number of social factors. (It is not entirely acceptable to use terms such as ‘second generation’, but the alternatives are cumbersome and even less palatable.) Although the new arrivals have their own set of problems, they also share problems with those who have been settled in the country for a considerable time.
Two hypotheses have been put forward to explain the relationship between migration and psychopathology – selection and stress. The selection hypothesis indicates that those who are vulnerable to mental illness (or already ill) tend to migrate. In contrast, the stress hypothesis suggests that psychosocial stressors related to migration are implicated in mental illness. A key aspect of this stress is related to social isolation and loss of social status, loss of social networks and is further complicated by acculturative processes. Goal-striving and additional high expectations may be shattered, thereby lowering the individual's self-esteem and intensifying stress.
Immigrant groups are exposed to similar stressful experiences as those of majority groups, but the responses may well vary owing to migratory stressors (pre- and post-migration), personality, past experiences, social networks, family support and other vulnerability and protective factors. There are social factors that appear to be significant in their impact on an individual's well-being – these include housing, employment, socio-economic status and social networks. There is little doubt that unemployed individuals are more likely to have poor self-esteem, low socio-economic status and perhaps less than ideal social networks. Unemployment has been closely linked with poor physical and mental health. Similarly, poverty and poor housing are related to aetiological factors in the onset of schizophrenia.
Recent work on social capital, defined as social cohesion and trust at a community level, shows that it is associated with psychosocial risk (Reference WilkinsonWilkinson, 1999). Social status and affiliations, and inequalities of power, income and status, are considered risk factors, while supportive social relations are considered protective. Such risk factors are shown to operate on the risk of mortality and community crime, including homicide. These can be considered as manifestations of extreme community distress and, if operative for African–Caribbean groups in the UK, might explain some vulnerability. It is known that early childhood environments and the quality of peer and attachment relationships are predictive of adult risks of ill health (Reference WilkinsonWilkinson, 1999). If African–Caribbean people born in Britain are exposed to a particular social environment in which they suffer exclusion, low social status, an internalised sense of inferiority and disadvantage in adulthood, then such influences might explain a higher risk of adult psychological distress. However, there are few data directly linking the risk of schizophrenia to social capital or to the childhood experience of relationships, attachment and identity, other than data showing that Black children internalise projected prejudicial stereotypes. The question of why first-generation African–Caribbean people, rather than other immigrant minority groups, are especially at risk also requires more research.
As noted above, for African–Caribbeans, Bhugra et al (1997) found that rates of unemployment were much higher among the patients compared with the general population from the same ethnic background. They were also more likely to have been living alone, with low social support and poor confiding. African–Caribbean males were more likely to have been separated from their fathers for longer than 4 years. These findings appear to fit with the social capital literature, but any assertions need careful empirical work. Without it, as historical experience shows, stereotypes may be reinforced, to the detriment of African–Caribbean groups.
Racism
Racism and psychiatry have been associated in the minds of ethnic minorities as well as the general public largely because psychiatry and psychiatrists are seen as controlling and oppressive. Misdiagnosis, as well as mismanagement, is perceived to explain the increased rates of schizophrenia, as well as increased rates of detention under compulsory orders. This equating of misdiagnosis with racism requires some careful analysis. Racism can be an institutional practice that disadvantages particular groups, or it can consist of the damaging ignorance or prejudicial attitudes of individuals. At one level, all forms of disadvantage owing to professional intervention among African–Caribbean groups can, if racism is defined by a detrimental outcome, be considered racist. Institutional practices can lead to both over- and underdiagnosis. The problem of only invoking racism (individual or institutional) is that scrutiny is not given to the precise sets of relationships, motivations and practices that should be explored further. Direct racism in the form of racial harassment or traumatic life events that are linked to the sufferer's racial, ethnic or cultural origins do not, of course, cause schizophrenia, but they are serious life events that are, by definition, experienced by Black and other ethnic minorities. Life events are known to increase the risk of relapse, and they can be compounded by the stresses of poor social situation, housing or unemployment.
All mental health institutions should endeavour to understand institutional racism, as it may be an added burden that African–Caribbean people with schizophrenia have to bear. It is also likely that racist assumptions and behaviours affect some vulnerable individuals more than others, and combining these in a clinical assessment of cultural, individual-identity and self-esteem-related factors will help us develop an aetiological and conceptual model of schizophrenia better suited to African–Caribbean groups.
Population density
One of the possible explanations for differential rates of schizophrenia may be ethnic density. Faris & Dunham (1960) showed that individuals with schizophrenia were more likely to be living alone with smaller numbers of individuals from their own ethnic background around them. It is possible that, in cultures and societies that are largely sociocentric, an individual living alone in an isolated setting may develop phenomena that a psychiatrist considers to be psychosis in response to distress; in an individual living in proximity to others from the same background, the distress might manifest in a non-psychotic form. Murphy (1968) postulated that there are lower rates of psychiatric disorders among the foreign-born in those countries where immigrants constitute a larger proportion of the population. This may well explain lower rates of schizophrenia in Asian samples from Southall in west London, where the Asian population forms nearly 50% of the total (Reference Bhugra, Leff and MallettBhugra et al, 1997), but may also explain high rates reported by King et al (1994) in north London. Kraus (1969) too demonstrated a highly significant negative correlation between the rate of schizophrenia and the size of the particular immigrant group.
We postulate that, rather than size alone, it is population density on the one hand and social isolation, trust in the community and low self-esteem on the other that may contribute to the aetiology. As we previously demonstrated (Reference Bhugra, Mallett and LeffBhugra et al, 1999), longer periods of separation from one or both parents may lead to problems in adult attachment that affect patient compliance. Furthermore, low self-esteem may well act as an intermediary factor in affecting the individual's self-concept, adding to a sense of loneliness and isolation, as illustrated in Fig. 1. In this sense, for African–Caribbeans, living in Britain may generate distress by influencing their self-esteem, identity and chances of success. Schizophrenia, although understood as a predominantly genetic condition among Whites, may be seen as a label we give to the same syndromal pattern, but it may actually have different aetiological factors and prognosis in this group.
There is no doubt that schizophrenia has a multi-factorial aetiology. It is possible that some factors are more loaded and therefore more significant than others, and here ethnicity and implicit racism may also play a role. This model remains a hypothetical one and needs to be confirmed in large multi-centre studies with large numbers of various ethnic groups. For example, the sequence in which factors operate, and the relative contribution they make to the total risk of schizophrenia, require more research.
Conclusions
There is little doubt from the literature that rates of schizophrenia among African–Caribbeans are much higher in the UK when compared with Whites, although findings on comparison with other ethnic groups are equivocal. Some of the increase can be explained as a result of poor housing, high rates of unemployment and social isolation. An interactional model needs to be evaluated by empirical study of a number of factors, both environmental and psychological.
Multiple choice questions
-
1. Inception rates of schizophrenia in African–Caribbeans in the UK:
-
a are higher in the older generation
-
b are due solely to cannabis use
-
c are higher in the second generation
-
d are higher in siblings of the second generation
-
e are always the same as those among Asians.
-
-
2. Rates of schizophrenia among African–Caribbeans are:
-
a influenced by genetic factors alone
-
b have nothing to do with social class
-
c can be lowered by primary prevention
-
d are due to high rates of unemployment alone
-
e are owing to misdiagnosis alone.
-
-
3. Social factors shown to be associated with high rates of schizophrenia in African–Caribbeans are:
-
a unemployment
-
b poor housing
-
c migration
-
d social status
-
e higher education.
-
-
4. Misdiagnosis by psychiatrists:
-
a can explain away high rates
-
b is owing to misunderstanding of some phenomena
-
c never occurs in the UK
-
d can be eliminated to some extent
-
e is due to cultural stereotyping.
-
-
5. The assessment of patients with schizophrenia: a must take into account cultural factors
-
a must take into account cultural factors
-
b must include third-party information as far as possible
-
c must be culturally appropriate
-
d does not include physical assessment
-
e does not include baseline investigations.
-
Table 1 Summary of early studies from the USA
| Admission rates | Admission rates for schizophrenia | ||||
|---|---|---|---|---|---|
| Blacks | Whites | Blacks | Whites | Ratio | |
| McLean (1949) | 173 | 110 | 1.6:1 | ||
| Frumkin (1954) | 80 | 43 | 19 | 8 | 2.3:1 |
| Faris & Dunham (1960) | 41 | 33 | 1.3:1 | ||
| Jaco (1960) | 53 | 80 | 31 | 38 | 0.68:1 |
| Malzberg (1963) | 340 | 174 | 112 | 49 | 2.2:1 |
| Klee et al (1967) | 1950 | 1650 | – | – | 1.18:1 |
| Wilson & Lantz (1967) | 105 | 48 | 22 | 7 | 3:1¤ |
Table 2 Rates of schizophrenia in Africa-Caribbeans in the UK (per 1000) (modified from Bhugra, 2001)
| Study | Location | Diagnosis | Age std | White | A–C | Ratio1 |
|---|---|---|---|---|---|---|
| Hemsi (1967) | Camberwell (London) | Case notes | Yes | 3.0 | 13.0 | 4.0 |
| Cochrane (1977) | England & Wales | MHE data | Yes | (m) 8.7 | 29.0 | 3.3 |
| (f) 8.7 | 32.3 | 3.7 | ||||
| Carpenter & Brockington (1980) | Manchester | Hospital | Yes | 2.0 | 11.0 | 5.5 |
| Dean et al (1981) | South East | Own | Yes | (m) 1.1 | 5.5 | 5.0 |
| England | (f) 1.0 | 5.3 | 5.3 | |||
| Littlewood & Lipsedge (1981) | Hackney (London) | Own | Yes | 2.0 | 5.0 | 2.5 |
| McGovern & Cope (1987) | Birmingham | Hospital | Yes | (16–29) 1.4 | 11.7 | 8.4 |
| (30–64) 1.1 | 4.7 | 4.3 | ||||
| Harrison et al (1988) | Nottingham | Own | Yes | (16–29) 2.0 | 29.1 | 14.6 |
| (30–44) 1.6 | 19.7 | 12.3 | ||||
| Cochrane & Bal (1989) | England & Wales | MHE data | Yes | (m) 1.2 | 3.9 | 3.3 |
| (f) 1.2 | 3.3 | 2.8 | ||||
| Castle et al (1991) | London | Case notes | 1965–692 0.88 | 4.6 | 5.3 | |
| 1970–742 0.98 | 7.9 | 8.2 | ||||
| 1980–842 1.20 | 5.08 | 4.0 | ||||
| Thomas et al (1993) | Manchester | Hospital | Yes | 3.5 | 32.5 | 9.2 |
| Harrison et al (1997) | Nottingham | Own | Yes | 5.7 | 46.7 | 8.2 |
| Bhugra et al (1997) | London | PSE | Yes | 7.5 | 14.7 | 2.0 |
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | F | a | T | a | F | a | T |
| b | F | b | F | b | T | b | T | b | T |
| c | T | c | F | c | F | c | F | c | T |
| d | T | d | T | d | T | d | T | d | F |
| e | F | e | F | e | F | e | T | e | F¤ |
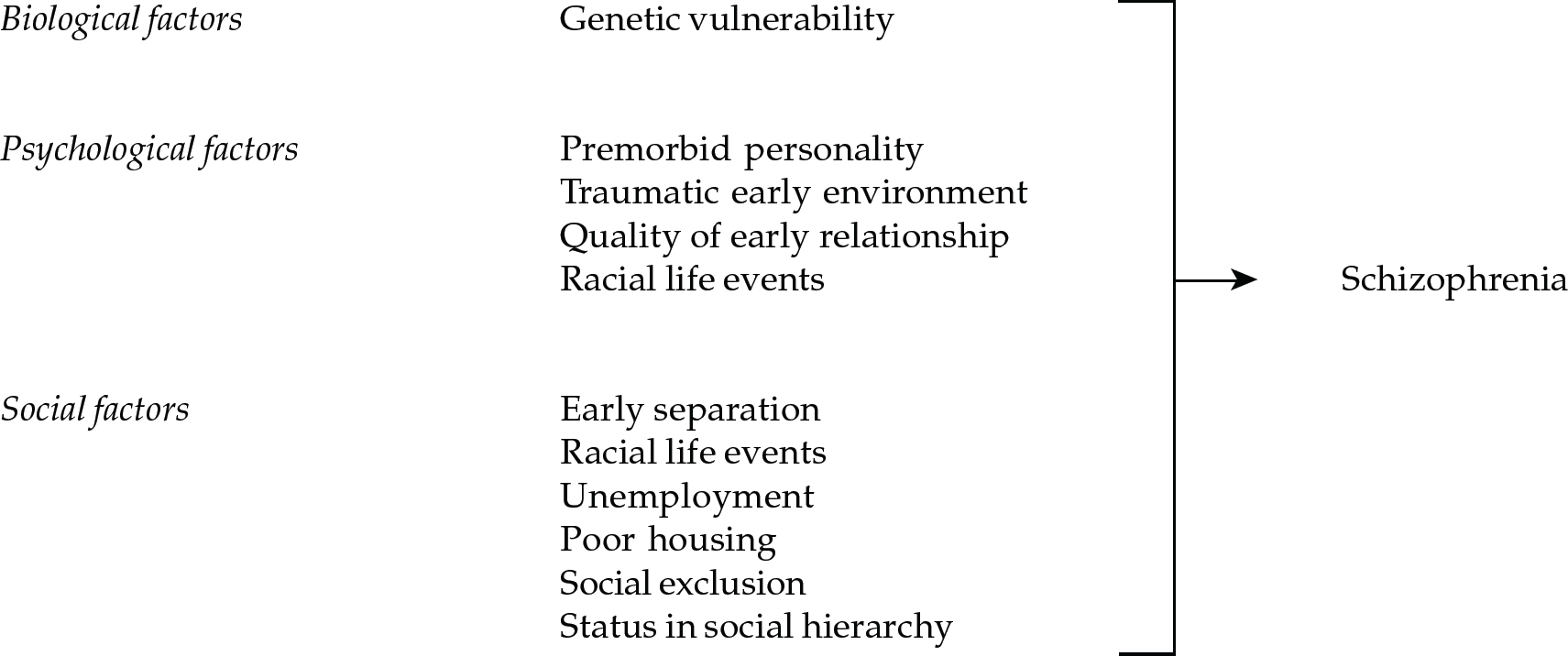
Fig. 1 A proposed model of aetiological factors requiring empirical evaluation








eLetters
No eLetters have been published for this article.